Approach to Interpreting Abdominal and Pelvic Magnetic Resonance Imaging Examinations
Many radiologists and radiology trainees are intimidated by the prospect of interpreting abdominal and pelvic magnetic resonance imaging (MRI) studies, but such fear is unfounded. We remind our residents and fellows of two reassuring facts. First, the anatomy of the human body does not change with changes in imaging modality or scan plane. Second, the diseases of the human body remain the same, no matter how they are imaged. The pancreas is in the same location on a coronal MRI scan as it is on an axial computed tomography (CT) scan, although it is displayed differently. Likewise, there is a limited differential diagnosis for a cystic pancreatic mass, regardless of the modality used to image it.
Individuals new to abdominal and pelvic MRI should adopt a systematic approach. When faced with an abdominal or pelvic MR image, we recommend going through the following checklist:
Is the image T1- or T2-weighted? A T2-weighted image is easily identified by the presence of high signal intensity fluid within the spinal canal, bile ducts, or urinary tract. Using the signal intensity of fat to distinguish a T1- from a T2-weighted image is not recommended.
If the image is T1-weighted, is it in-phase or out-of-phase? This applies to gradient echo images. An out-of-phase image demonstrates phase cancellation at fat-water interfaces, resulting in a characteristic dark rim around the solid organs.
Is the image fat-suppressed or non-fat-suppressed?
Which direction is phase-encoded and which is frequency-encoded? This is important because one needs to be able to distinguish phase ghosts and other artifacts from actual lesions within the abdomen.
Are any artifacts present? Initially looking for artifacts such as phase ghosting, wraparound, and susceptibility artifact may prevent misinterpreting such artifacts later in the interpretive process.
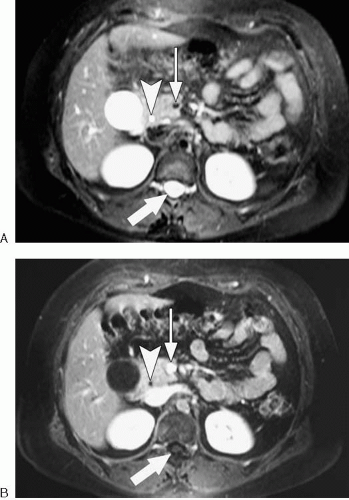
Has intravenous contrast been administered? A fat-suppressed, T1-weighted, contrast-enhanced image may look similar to a fat-suppressed T2-weighted image (Fig. 3.1).
For contrast-enhanced images, what is the phase of enhancement (e.g., arterial, venous, equilibrium, delayed)?
When an abnormality is seen, we recommend the following considerations:
In what organ or anatomic compartment is the abnormality located?
In which direction are adjacent organs or structures displaced?
Between what structures does the abnormality occur?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree