A good understanding of anorectal physiology is essential for the diagnosis and appropriate treatment of various anorectal disorders, such as fecal incontinence, constipation, and pain. This article reviews the physiology of the anorectum and details the various investigations used to diagnose anorectal physiology disorders. These anatomic and functional tests include anal manometry, endoanal ultrasound, defecography, balloon expulsion test, magnetic resonance imaging, pudendal nerve terminal motor latency, electromyography, and colonic transit studies. Indications for investigations, steps in performing the tests, and interpretation of results are discussed.
Key points
- •
Anorectal physiology involves muscle and nervous coordination to ensure controlled and timely bowel movements.
- •
The understanding of anorectal physiology is essential so that the physician may order appropriate testing to elicit the most useful information to guide the diagnosis and treatment of anorectal disorders, such as fecal incontinence, constipation, and pain.
- •
Digital rectal examination should be performed to gain information about a patient’s anorectal physiology and to guide investigations.
- •
Anal manometry, endoanal ultrasound, defecography, balloon expulsion test, magnetic resonance imaging, colonic transit studies, pudendal nerve terminal motor latency studies, and electromyography are commonly used in testing anorectal physiology and are ordered as appropriate based on the patients’ symptoms.
Introduction
The processes of defecation and maintenance of fecal continence are complex, involving both voluntary and involuntary muscular activity. The pudendal and sacral nerves provide important sensory and motor information. The rectum functions as a distensible reservoir to permit time control over the evacuation of stool. All of these activities and anatomic units must act in concert for effective defecation. When there is dysfunction, various disorders may result. These disorders include fecal incontinence, constipation, obstructed defecation, pelvic pain, and the symptoms of ineffective defecation, such as incomplete evacuation or clustered frequent bowel movements.
These disorders have major impacts on the daily life of patients. Patients may, for example, be unable to work because of pain or avoid social activities because of fecal incontinence. The morbidities of these conditions are wide reaching, and the proper treatment may have just as powerful of an effect on patients’ lives. Anorectal testing is used to discern the most effective potential treatments for an individual patient. The anorectal investigations described in this article are not all available in every institution. Specialized equipment is needed for nearly all of the tests, as are educated health care professionals to both perform the tests and interpret the results. For a fully comprehensive anorectal physiology program, expertise may be used from colorectal surgery, gastroenterology, radiology, and neurology. Although much of the anorectal physiology testing may be office based, an equipped radiology department is needed for tests, such as defecography and magnetic resonance imaging (MRI).
Anorectal testing can be divided into anatomic and functional tests, with some overlap. The anatomic tests include endoanal ultrasound, defecography, and MRI. Functional tests include anal manometry, balloon expulsion test, defecography, dynamic MRI, colonic transit studies, pudendal nerve terminal motor latency study, and electromyography. Each test is described later.
Introduction
The processes of defecation and maintenance of fecal continence are complex, involving both voluntary and involuntary muscular activity. The pudendal and sacral nerves provide important sensory and motor information. The rectum functions as a distensible reservoir to permit time control over the evacuation of stool. All of these activities and anatomic units must act in concert for effective defecation. When there is dysfunction, various disorders may result. These disorders include fecal incontinence, constipation, obstructed defecation, pelvic pain, and the symptoms of ineffective defecation, such as incomplete evacuation or clustered frequent bowel movements.
These disorders have major impacts on the daily life of patients. Patients may, for example, be unable to work because of pain or avoid social activities because of fecal incontinence. The morbidities of these conditions are wide reaching, and the proper treatment may have just as powerful of an effect on patients’ lives. Anorectal testing is used to discern the most effective potential treatments for an individual patient. The anorectal investigations described in this article are not all available in every institution. Specialized equipment is needed for nearly all of the tests, as are educated health care professionals to both perform the tests and interpret the results. For a fully comprehensive anorectal physiology program, expertise may be used from colorectal surgery, gastroenterology, radiology, and neurology. Although much of the anorectal physiology testing may be office based, an equipped radiology department is needed for tests, such as defecography and magnetic resonance imaging (MRI).
Anorectal testing can be divided into anatomic and functional tests, with some overlap. The anatomic tests include endoanal ultrasound, defecography, and MRI. Functional tests include anal manometry, balloon expulsion test, defecography, dynamic MRI, colonic transit studies, pudendal nerve terminal motor latency study, and electromyography. Each test is described later.
Anorectal physiology
Anorectal physiology is complex. It involves the pelvic floor muscles, motor and sensory neural pathways and is intimately related to the colon physiology. Maintenance of continence depends largely on the pelvic floor musculature, which reacts to signals related to stool consistency and overall bowel motility.
Sensory Physiology
The anal canal receives sensory input from the S2, S3, and S4 nerve roots; composing the pudendal nerve. Although the rectum is only sensitive to stretch, the anus is sensitive to temperature, touch, and pain. These sensations may help a person to assess when it is inconvenient to evacuate stool from an environmental perspective. This area of sensation represents the anal canal, which is kept closed at rest mainly by the internal sphincter muscle.
When the rectum senses stool or flatus, the sensory mechanism allows the rectum to be compliant and stretch to accommodate stool. This sensation should not be a painful sensory response and, in fact, will alleviate the discomfort of the sensation of urgency. Once rectal distension has reached a threshold of compliance, anal canal sensory reflexes result in relaxation and evacuation of stool. The relationship between rectal sensation and anal canal sensation exists but is not essential to maintain continence. For example, most patients with colonic or ileal pouches are able to maintain continence despite not having a rectum to signal to the anal canal.
Motor Physiology
The main muscles to consider in anal physiology, namely, the maintenance of continence and effective defecation, are the internal sphincter, external sphincter, and puborectalis muscles. The sphincters are not paired to each other and have distinct functions. The internal anal sphincter is an involuntary muscle. It is innervated by the hypogastric and pelvic plexi and contributes to more than 50% of the resting anal tone. It plays a vital role in continence. At rest, a basal tone of the internal sphincter is maintained by slow, constant waves of contraction. During defecation, the internal sphincter involuntarily relaxes to allow for the evacuation of stool.
The external anal sphincter contributes 30% of the resting tone, with hemorrhoidal tissue contributing the remaining 15%. It contains mainly striated type I fibers muscle, which allows the maintenance of a baseline tone at rest. It is innervated by the pudendal nerve. A baseline level of tone is maintained at rest. Voluntary contraction may be performed to increase tone and hold in flatus or stool and can last up to 1 minute before the muscle fatigues. During evacuation, voluntary relaxation of the external anal sphincter occurs to permit the passage of stool and flatus.
The puborectalis is a striated muscle that inserts into the pubis and acts as a sling for the rectum. This sling effect creates the anorectal angle at rest, which helps to limit the volume of stool passing into the distal rectum and anal canal. During defecation, the puborectalis relaxes and lengthens, allowing the rectum to straighten and stool to move into the distal rectum and anal canal for evacuation. If paradoxic contraction or nonrelaxation occurs, patients may experience pain, constipation, and incomplete evacuation. Along with the internal and external anal sphincters, the puborectalis is an identifiable anatomic landmark when performing endoanal ultrasound.
There are numerous anorectal reflexes. These reflexes are summarized in Table 1 .
| Name | Reflex | Notes |
|---|---|---|
| Rectoanal inhibitory reflex | Internal anal sphincter muscle relaxation caused by rectal distension |
|
| Cutaneous anal sphincter reflex | Contraction of the distal external sphincter muscle with touch or pain stimulus of anal skin |
|
| Bulbocavernosus reflex | Contraction of external anal sphincter muscle with squeezing the glans penis or clitoris or pulling on urethral catheter |
|
| Cough-anal reflex | Contraction of the external anal sphincter muscle in response to coughing or sniffing |
|
Anorectal testing
The tools used to investigate anorectal disorders include both anatomic and functional testing. Not every test is necessary for each patient or each disorder. Investigations should be ordered based on the following:
- •
Complete history and physical examination
- •
Digital rectal examination
- •
Review of previous investigations and consultations
- •
Stool diary when appropriate
General indications for each of the anorectal tests discussed in this article are summarized in Table 2 .
| Test | Potential Indications |
|---|---|
| Anal manometry | Fecal incontinence Constipation Hirschsprung Anal fissure Anal pain |
| Endoanal ultrasound | Fecal incontinence Constipation Sphincter defect Anal Fistula Anal pain |
| Defecography | Constipation Fecal incontinence Obstructed defecation Pelvic descent Suspected prolapse Suspected rectocele Anal pain |
| MRI | Constipation Fecal incontinence Obstructed defecation Pelvic descent, multiple compartments Sphincter defect Suspected rectocele Anal pain |
| Balloon expulsion test | Obstructed defecation Constipation |
| Pudendal nerve terminal motor latency | Fecal incontinence Constipation Suspected nerve injury |
| Electromyography | Fecal incontinence Suspected nerve injury Constipation |
| Colonic transit study | Constipation Obstructed defecation |
Digital Rectal Examination
Although not an anorectal physiology test or investigation , special mention must be given to the utility of a digital rectal examination. It is an essential portion of the physical examination for an anorectal problem. The components of a digital rectal examination are listed in Box 1 . Digital rectal examination should be performed in a systematic fashion to gather the most useful information. Patients should be placed ideally in a prone kneeling position on an examination table that may be raised and tilted to permit the best view of the anorectum. If this is not available, patients should be positioned in the lateral decubitus position.
- •
Inspection
- •
Digital examination
- •
Anoscopy
The digital rectal examination should begin with inspection of the perianal skin for rashes, skin changes, scars, external skin tags, fissure, and evidence of active infection, such as induration or drainage. While inspecting, patients should be instructed to squeeze the sphincter muscles. A perianal wink should be visualized. Perianal sensation can be tested using a pinprick method when indicated. Patients should be instructed that a lubricated finger will be inserted into the anus. Initial contact with the perianal skin should produce a visible involuntary reflex. Digital examination should be performed to the full length of the finger if tolerated by the patients. The clinician should feel for bulky internal hemorrhoids, prostate, ulceration, and mass. With the finger inserted, resting and squeeze tone should be tested by asking patients to squeeze and relax the anal sphincters. Paradoxic contraction may be assessed by having patients valsalva while the finger is inserted and noting the presence of abnormal sphincter contraction around the finger. Anoscopy may be performed if indicated. This examination allows for the visualization of the anal canal and hemorrhoid columns. Occult blood testing may be performed if there is a concern for rectal bleeding by using fecal material from the gloved finger.
The digital rectal examination may help diagnose anorectal disorders and guide other anorectal testing. In women with constipation and incomplete evacuation, clinical examination with digital rectal examination revealed hypertonic sphincters or rectoceles in 40% of cases. Digital rectal examination, when compared with physiology tests, is accurate in the assessment of sphincter function but should not be used to solely diagnose sphincter defects. The overall sensitivity and specificity of digital rectal examination in evaluating normal resting and squeeze tone has been shown to be more than 75% and is accurate in detecting rectoceles. It should always be the starting point for the assessment of anorectal physiology and function.
Anal Manometry
Manometry is a functional test that assesses the tone and function of the anal sphincter muscles. It is performed in the office or physiology laboratory with awake patients. Manometry is useful in the assessment of both fecal incontinence and constipation because it provides a measure of the effectiveness of the anorectal musculature, the rectoanal inhibitory reflex, sensation, and compliance of the rectum. Variations in technique are used to assess these functions, namely, the pull-through or stationary techniques. Newer variations using 3-dimensional measurements and high-resolution technologies are being developed to improve the utility of manometric results. The authors’ preference is the pull-through technique.
When using anal manometry in one’s practice, it is important to note that normal values vary between patient groups. Women have lower resting and squeeze pressures when compared with men. Younger women have resting and squeeze pressure that approach those of men, especially nulliparous young women. Accurate and useful results depend on having a trained operator for the equipment and consideration of patient age and gender.
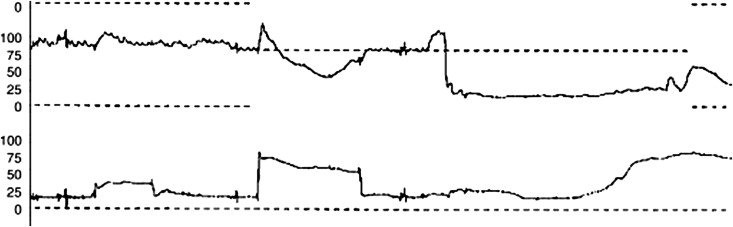
To perform an anal manometry, patients are positioned in the left decubitus position. Digital rectal examination is performed to ensure there is no obstruction before inserting the catheter. A manometry probe with a deflated latex balloon at the tip is calibrated to the machine at the level of the anus. The probe is inserted to a distance of 6 to 10 cm and held at that level using a mechanical arm and left in place for 30 seconds before attaining any measurements. Resting and squeeze pressures are measured 3 times each, and mean pressures are calculated. Each squeeze pressure is measured for a sustained squeeze period of 30 seconds. A small volume of water is instilled into the balloon for the measurement of first sensation, typically between 20 and 60 mL of water. Compliance is measured by instilling further water into the balloon until not tolerated by patients, with normal compliance being between 100 and 200 mL of water. The water is then removed. A small volume of air, about 20 mL, is instilled into the balloon over 1 to 2 seconds to elicit a rectoanal inhibitory reflex by a characteristic manometric curve seen on the screen. If the reflex is absent, the process is repeated using 10 mL of more air each time up to the volume of first sensation to see if the reflex is present. Fig. 1 shows the pressure curve of a normal rectoanal inhibitory reflex.