Fig. 3.1
Embryonal development of the cloaca (Reproduced from Schunke M, et al. Promethius LernAtlas der Anatomie, vol. 2. 3rd ed. Stuttgart: Thieme Publ.; 2012, with permission)
At this point the urorectal septum and proctodeal membrane become the perineal body and overlying skin and the now separated anterior and posterior portions of proctodaeum, fused with cloacal endoderm, become the urogenital membrane and anal membrane respectively. These membranes indent and become the urogenital sinus and anorectal canal at about the seventh week of gestation. The anorectal membrane perforates by degeneration leaving a differentiation gradient from rectal columnar epithelium through to squamous keratinised epithelium within the anal canal. This corresponds to the region of mucosa just above the dentate line.
The embryology of the urogenital sinus and ventral attachments to the cloaca account for the proximity of the genital structures, and their neurovascular supply, to the anorectum – in particular the posterior vaginal wall in the female and seminal vesicles and prostate in the male. It is therefore important to understand the embryology and anatomy of these structures when considering the need for oncologically beneficial surgery and its potential effects on sexual and urinary function.
Oncological principles regarding rectal cancer surgery derive from the fact that the blood supply and lymphatic drainage of almost the entire rectum are visceral, via the superior rectal artery, and associated lymphatics, from the hindgut originator vessel, the inferior mesenteric artery. The lymphovascular supply is encased, as are all mesenteries, in a fascial layer. In the case of the mesorectum this capsule is termed the mesorectal fascia and constitutes part of the endopelvic fascia. The mesorectal fascia separates the visceral rectum from the somatic pelvis but also from the fascial septum of the genital organs – the rectovaginal septum in females and Denonvilliers fascia in males.
Anatomy of the Rectum
The rectum is the last absorptive and propulsive part of the gastrointestinal tract and bridges the last 15–20 cm of gut from sacral promontory to anal orifice, its mesentery wrapped in mesorectal fascia, lying anterior to the sacral concavity, superior to the anal hiatus of the pelvic floor muscles, posterior to the rectovaginal septum vagina and uterus/ Denonvilliers’ fascia, prostate seminal vesicles and bladder. The anal canal lies at a dorsal angle of 90–100° to the rectum due to tonic contraction of the puborectalis muscle of the pelvic floor. This is known as the anorectal angle.
The rectum can be divided functionally and anatomically into two parts: the upper part being mainly propulsive and sharing a similar diameter to the sigmoid above; the lower part, being mainly for storage, is dilated, sometimes considerably, to form the rectal ampulla. The rectum is recognisably different from the colon at surgery due to the absence of appendices epiploicae and the diffusion of longitudinal muscle bands (teniae coli) to form a continuous longitudinal smooth muscle layer.
The upper two thirds of the anterior rectal wall are covered by peritoneum. The rest of the rectum and its mesorectal package are retro/extraperitoneal. The pelvic peritoneum covering the rectum thickens and reflects laterally and anteriorly to cover the ureters, endopelvic fasciae, posterior bladder and seminal vesicles and prostate in the male (the rectovesical pouch). The pelvic peritoneum covers the uterus and fallopian tubes (the broad ligament), posterior cervix and posterior vaginal fornix in the female (rectouterine pouch of Douglas). It is continuous with the parietal peritoneum of the anterior abdominal wall.
Blood Supply to the Rectum
The visceral blood supply to the rectum is from the inferior mesenteric artery via the superior rectal artery dividing into mesorectal branches and comprises at least 80 % of the rectal blood supply. The mesorectal branches further ramify from posterior to lateral and anteriorly perforating the muscle layers of the rectal wall to supply the muscles, submucosa and mucosa. They descend in the muscle and submucosal layers towards the upper anal canal.
These mesorectal arteries anastomose at capillary level with supply from the middle rectal arteries which are branches of the internal iliac arteries to supply that portion of the rectum passing through the pelvic floor. They are inconsistently present and are only bilaterally detectable as distinct vessels in 10 % of individuals. They pass with rectal branches of the inferior hypogastric nerve plexi in fascial condensations commonly, but not universally, recognised as the “lateral ligaments”.
Below the pelvic floor the remainder of the blood supply to the anorectum is from the superior haemorrhoidal (also known as the inferior rectal) arteries which, passing through the ischioanal space, are branches of the internal pudendal arteries which pass through Alcock’s canal, themselves branches of the internal iliac arteries. Thus there is a connection between visceral and somatic blood supplies – inferior mesenteric and internal iliac.
Venous Drainage of the Rectum
Via multiple veins within the mesorectum most blood drains to the inferior mesenteric vein (IMV) which drains into the splenic vein behind the pancreas. The IMV is seen within the descending colonic mesentery passing behind the pancreas at the level of the ligament of Treitz at the duodenojejunal flexure. The blood then enters the portal venous system and it is thought that hepatic metastases arise by haematogenous spread via this route.
There is a rich network of venous connections within the mesorectum, however, and some of the rectal blood supply also drains via the inferior rectal veins to the internal iliac veins. It is thought that via this route distant extrahepatic metastases (e.g. lung) arise by haematogenous spread.
Operative Significance
The inferior mesenteric artery is divided close to its origin from the aorta at curative rectal cancer surgery taking care to avoid damaging the hypogastric nerve plexus. This often results in taking the ascending left colic branch which supplies the descending colon and anastomoses variably with the marginal artery from the distal branches of the middle colic arteries supplying the transverse colon, whose origin is the superior mesenteric artery (SMA). Once the specimen is resected the residual colon to be anastomosed to the anorectum at the pelvic floor can therefore be considered a pedicled flap, whose sole blood supply is then the marginal artery.
The IMV can cause significant tethering of the colonic pedicle if not divided high near the ligament of Trietz. This manoeuvre is important in ensuring a tension free coloanal anastomosis.
It is thanks to the multiplicity of blood supply to the lowermost anorectal muscle and mucosa that coloanal anastomoses are possible. Thus marginal arterial supply from the SMA meets pudendal arterial supply from the internal iliac arteries to perfuse the healing anastomosis.
Lymphatic Drainage of the Rectum
Lymphatic drainage of the rectum is mainly in a cranial direction from the submucosa to mesorectal lymph nodes to inferior mesenteric lymph nodes and then para-aortic nodes. Thus typical patterns of lymph node involvement present themselves in cases of rectal cancer. However given the presence or absence of middle rectal vessels drainage to lateral pelvic sidewall or internal iliac nodes is also possible. Thus lateral pelvic lymph node metastases may also occur but tend to happen with more locally advanced mid to lower rectal cancers which have breached the circumferential mesorectal fascial margin.
Nerve Supply to the Rectum
The rectum is neurally supplied by the autonomic nervous system. This comprises an intrinsic (myenteric & submucosal) and extrinsic sympathetic and parasympathetic system. The intrinsic system consists of a network of nerve plexi and ganglia supplying the mucosa, submucosa and all muscle layers of the rectum. Responsive to stretch and chemical stimuli, the intrinsic system is chiefly responsible for motility, secretion, absorption, perception and immune function. These nerve plexi are linked to the central nervous system by autonomic sympathetic and parasympathetic nerves via ganglia to spinal visceral afferents.
The sympathetic nerves reach the rectum via the superior sympathetic pre-aortic, and inferior mesenteric plexi which condense to form the hypogastric bundle which then divides below the aortic bifurcation anterior to the sacral promontory into right and left hypogastric nerves. These then course laterally in the pelvis and join spinal parasympathetic nerves (pelvic splanchnic nerves), which exit the sacral foramina with sacral nerves 2, 3 and 4, to form the inferior hypogastric plexi, branches of which form the rectal plexus to supply the rectum on each lateral side through the aforementioned fascial condensations known as the lateral ligaments. The inferior hypogastric plexus then continues anteriorly as a condensation within neurovascular bundles to supply the urinary bladder and cavernous nerves of sexual function.
Fascial Layers of the Pelvis
The pelvis and its contents can be thought of as a series of concentric and eccentric fascial layers and spaces rather like an onion/shallot in which another eccentric allium has grown. Working from outside to in, the bony pelvis is covered in periosteum, a musculoaponeurotic layer including the iliopsoas, obturators, piriformis and pelvic floor muscles, nerve roots, somatic nerves of the lumbar and sacral plexi, and blood vessels including the iliac vessels and their branches. Anterior to the sacrum this layer is known as the pre-sacral space which contains areolar tissue and significant presacral veins which can be easily damaged causing massive haemorrhage without careful dissection in the correct plane.
This layer is then encased in the parietal pelvic fascia. Anterior to the sacral concavity this is known as presacral fascia. Laterally below the level of the peritoneal reflection this fascia invaginates centrally on either side toward the mesorectum to allow the passage of the rectal nerve plexi and middle rectal arteries (if present) to supply the rectal wall. The posterior and anterior leaves of these fascial invaginations condense with the neurovascular bundles to form the “lateral ligaments” also described as rectal pedicles or “T junctions” (Fig. 3.2). They offer no support mechanism merely a conduit for neurovascular supply.
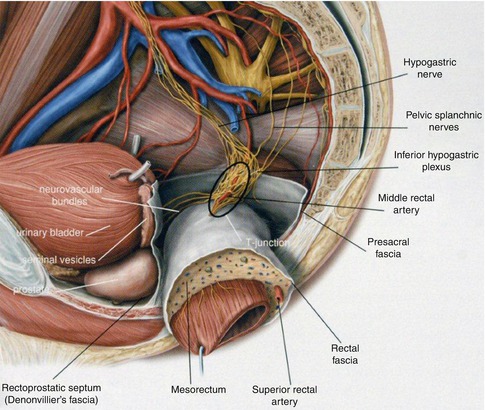
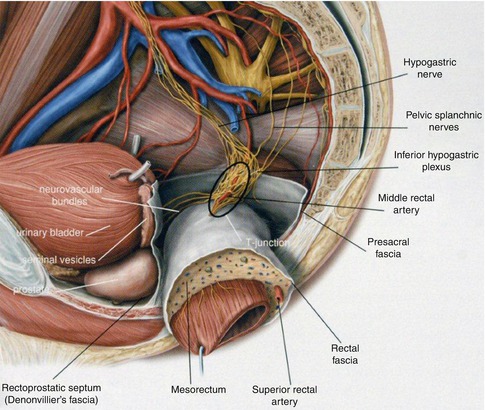
Fig. 3.2
Perirectal spaces, sagittal section of male pelvis, left view. The rectum and the surrounding mesorectum are pushed towards the contralateral side to illustrate the course of the autonomic pelvic nerves along the pelvic wall (Reproduced from Schunke M, et al. Promethius LernAtlas der Anatomie, vol. 2. 3rd ed. Stuttgart: Thieme Publ.; 2012, with permission)
Inferiorly the parietal pelvic fascia thickens over the pelvic floor musculature and is known as Waldeyer’s fascia (Fig. 3.3). Anterior to the rectum and posterior to the urogenital organs the parietal fascia overlies the perineal body and anterior and posterior leaflets of this fascia rise together fused between urogenital organs and anterior rectum forming a rectogenital septum to reach the most caudal portion of the peritoneum – the pouch of Douglas/rectovesical pouch. It continues laterally and is continuous with the lateral aspects of the presacral fascia. This condensation of fascia is of considerable density in its upper portions and can clearly be seen in two layers (Fig. 3.3) with the magnified views obtained at laparoscopic and robotic surgery, and histopathologically. However, inferiorly it is less distinct in the male and appears to fuse with the prostatic capsule. It is the embryological urorectal septum or rectogenital septum in the adult and as described before constitutes the rectovaginal septum in the female and Denonvilliers’ fascia in the male. (It can be severely damaged and rendered vestigial in females after childbirth. This contributes to the formation of rectocoeles.) It effectively divides the pelvis into anterior and posterior (anterior/middle and posterior in females) compartments from now on.
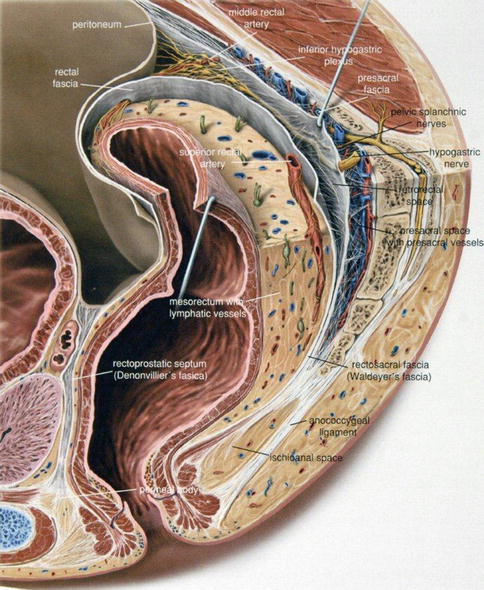
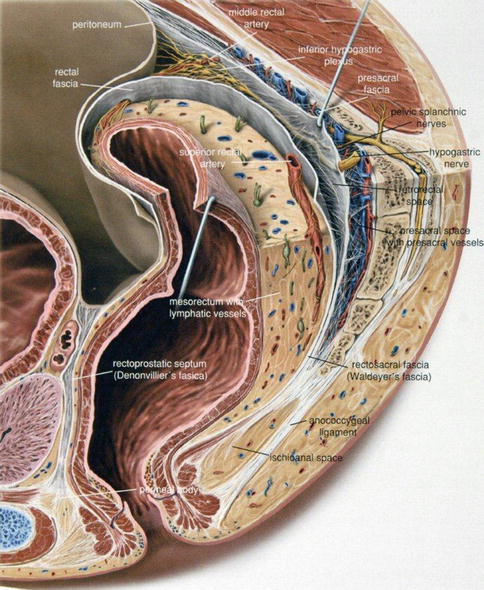
Fig. 3.3
Perirectal fascia, mediosagittal section of male pelvis, left view. The endopelvic mesorectal fascia and parietal pelvic presacral fascia are highlighted to illustrate the perirectal mesorectum and retrorectal and presacral spaces (planes). Of note the retrorectal space (“mesorectal plane”) is free of blood vessels and nerves and corresponds to the correct surgical plane for rectal mobilisation during total mesorectal excision (Reproduced from Schunke M, et al. Promethius LernAtlas der Anatomie, vol. 2. 3rd ed. Stuttgart: Thieme Publ.; 2012, with permission)
Posterior Compartment
Outer Layer 1 is the retrorectal space which contains the hypogastric nerves, inferior hypogastric plexi (and middle rectal vessels if present). These extrinsic autonomic nerves therefore all lie between peritoneum, parietal presacral fascia and mesorectal fascia covered by a flimsy fascial sheath (pre-hypogastric nerve fascia). This layer also contains the inferior posterolateral pelvic portions of the ureters and gonadal vessels.
Middle Layer 2 is the endopelvic visceral fascia of the rectum or mesorectal fascia. The mesorectum is wrapped around by the mesorectal fascia which is considerably more substantial posteriorly where under tension at surgery it can lead to the appearance of bilateral bulges.
It fuses with the parietal fascia at the lateral ligaments and at the level of S4 with Waldeyer’s fascia as it passes through the pelvic floor.
Inner layer 3 is the mesorectum and rectum itself.
Anterior Compartment
Outer Layer 1 contains the anterior pelvic portions of the ureters and gonadal vessels and vasa deferentia.
Middle Layer 2 is the endopelvic visceral fasciae of the urogenital organs. The fasciae are generally thin and flimsy. They include ureteric sheaths and gonadal vessel sheaths, perivesical fascia, and fascia overlying the prostate and seminal vesicles and vasa deferentia in the male, and vagina, cervix and uterus in the female. pelvic urogenital organs and related blood vessels.
Inner layer 3 contains the aforementioned urogenital organs.
The central lining layer of the pelvis is the pelvic peritoneum as described above.
Oncological and Functional Significance of the Mesorectal Fascia
It has been demonstrated that the quality of the resected specimen (intactness of the mesorectal fascia) and lack of tumour involvement of the circumferential resection margin are independent prognostic markers for local recurrence after rectal cancer resection. Thus a clear understanding and recognition of the mesorectal fascia and the surgically distinct avascular plane around it is essential for producing a complete specimen removal with an intact fascia for the success of surgery as the primary curative treatment for rectal cancer. Remaining in the correct plane between the mesorectum and parietal pelvic fascia and rectogenital septum facilitates identification of, and reduces the likelihood of damage to, the neurovascular structures important in maintaining normal urogenital function. These are therefore the principles by which the total mesorectal excision (TME) was popularised.
Tumours which lie within 1 mm of the mesorectal fascia are considered “circumferential resection margin-positive” so even with an optimal surgically resected specimen there is a high risk for local recurrence in these cases. It has also been shown that high resolution preoperative imaging in the form of MRI has helped to predict a threatened CRM by recognition of the mesorectal fascia and the proximity of such tumours. In these cases, as part of a multidisciplinary appraisal, selective neoadjuvant treatment in the form of chemoradiotherapy may be offered to patients to improve their risk of local recurrence.
Anatomy of the Anus
The rectal ampulla narrows at the level of the pelvic floor at the anorectal junction and becomes the upper anal canal which extends caudally and posteriorly towards the anal orifice. The anal canal is on average 3.5–5 cm long.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






