(1)
Department of Endoscopy, Fukuoka University Chikushi Hospital, Fukuoka, Chikushino, Japan
Abstract
In this chapter, I will present early gastric epithelial neoplasias (differentiated gastric cancer and adenoma), stratified for Paris classification of macroscopic appearance, and their characteristic magnifying endoscopy (ME) findings. I will explain how to read and interpret ME findings using the VS classification, with reference to the pathohistological findings. The Paris classification is usually applied to early gastric cancers, but for convenience’s sake I will use it for adenomas as well in this chapter. First table of this chapter shows the macroscopic classification of the presented cases and the characteristic ME findings I wish to highlight. In particular, I will summarize the ME findings of the “background mucosa,” “marginal area,” and “lesion” and add an explanation for each.
Keywords
AdenomaEarly gastric cancerMagnifying endoscopyParis classificationStomach13.1 Superficial Shallow Depressed Type (0 IIc)
13.1.1 Case 1: Typical IIc Type, IMVP Plus IMSP (Figs. 13.1– 13.5)

Fig. 13.1
On the lesser curvature of the gastric cardia we can see a depressed lesion with an irregular margin slightly raised on the inside
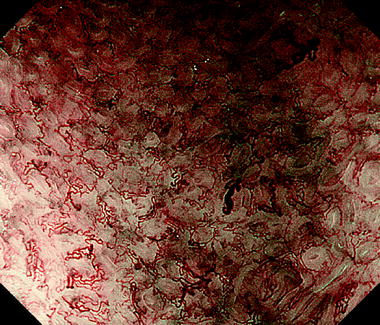
Fig. 13.2
Background mucosa
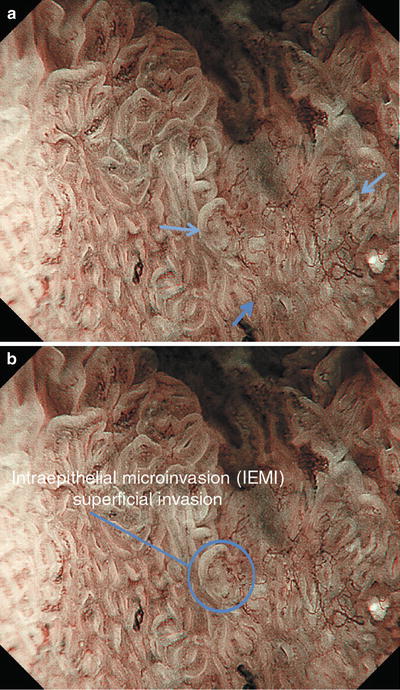
Fig. 13.3
(a, b) Marginal area
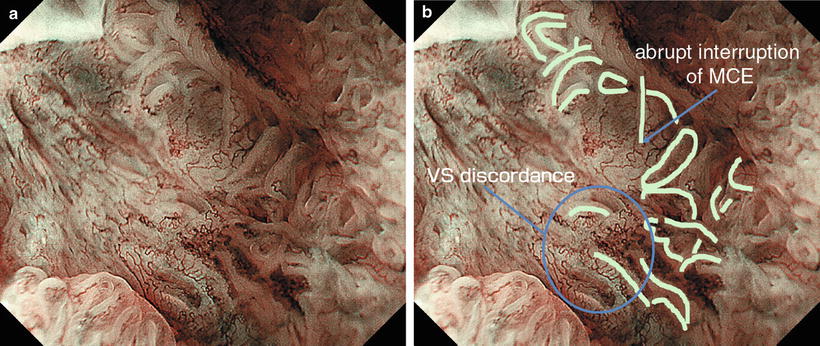
Fig. 13.4
(a, b) Lesion
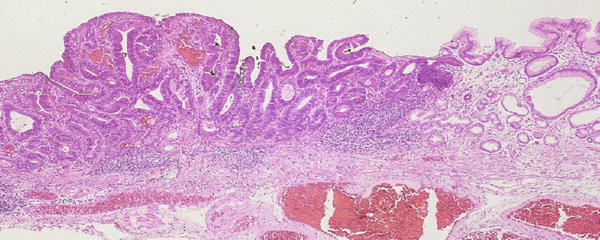
Fig. 13.5
Histological findings corresponding to the specimen in Fig. 13.4a, b. The clearly visible MCE in the marginal area is consistent with a well differentiated adenocarcinoma, arising from large atypical glands. This histological structure was visualized as an irregular section of MCE
Lesser curvature of the gastric cardia, 0 IIc type, differentiated type (well-differentiated adenocarcinoma), depth of invasion M, typical 0 IIc type on non-magnifying endoscopy, typical ME findings of early gastric cancer (EGC) (Table 13.1).
Table 13.1
List of cases stratified for Paris classification of macroscopic appearance and characteristic magnifying endoscopy (ME) findings
Paris classification | Case no. | Non-ME findings | Depth of invasion | Characteristic ME findings | MV pattern | MS pattern |
|---|---|---|---|---|---|---|
13.1. Superficial shallow depressed type (0 IIc) | 1 2 3 4 5 6 7 8 9 | Typical IIc Typical IIc Typical IIc Typical IIc Small IIc Micro IIc Typical IIc Depressed adenoma (1) Depressed adenoma (2) | M M M SM3 M M M | IMVP plus IMSP IMVP plus IMSP Irregular WOS IEMI MCE elements Irregular WOS Atypical cancer Typical adenoma Typical adenoma | Irregular Irregular Absent Irregular Irregular Absent Regular Regular Regular | Irregular Irregular Irregular Absent Irregular Irregular Regular Regular Absent |
13.2. Superficial flat type (0 IIb) | 10 11 | Typical IIb Minute IIb | M M | IMVP plus IMSP IMVP plus IMSP | Irregular Irregular | Irregular Irregular |
13.3. Superficial slightly elevated type (0 IIa) | 12 13 14 15 16 17 18 19 | Typical IIa Typical IIa Typical IIa Typical IIa Adenoma (1) Adenoma (2) Adenoma (3) Adenoma (4) | M M M SM1 | VS discordance IEMI IEMI, irregular WOS Irregular WOS Typical adenoma Typical adenoma Regular WOS Regular WOS | Irregular Irregular Irregular Absent Regular Regular Absent Absent | Irregular Irregular Irregular Irregular Regular Regular Regular Regular |
13.4. Polypoid type (0 I) | 20 | Typical I | M | IMVP plus RMSP | Irregular | Regular |
13.5. Lesions with a distinctive appearance on magnifying endoscopy | 21 22 | Typical IIa Typical IIc | SM3 SM1 | VEC pattern Villous carcinoma | Irregular Irregular | Regular Irregular |
13.1.1.1 Non-magnifying Endoscopy Findings (Fig. 13.1)
13.1.1.2 ME Findings (Maximal Magnifying Ratio, Water Immersion Technique)
Background mucosa
VS classification: regular MV pattern plus regular MS pattern
VS discordance: no
Marginal area
DL: present
IEMI: present (superficial invasion)
Lesion
VS classification: irregular MV pattern plus irregular MS pattern
VS discordance: yes
Background mucosa (Fig. 13.2)
V: Subepithelial capillaries form loops from small closed curves, overall linking up to make a regular honeycomb-like SECN.
S: The sections of MCE show a closed curved to crescentic structure, with a uniform width.
VS discordance: No dissociation of the V and S components is seen, so there is no VS discordance.
Marginal area (Fig. 13.3a)
As shown in Fig. 13.3a, in the cancer marginal area we can see a clear DL due to differences in the V and S components between the cancerous and noncancerous mucosa. Towards the anal side, there is little unevenness of the surface, and the arrows in Fig. 13.3a, and circle in Fig. 13.3b, indicate sites where the cancer (IMVP) invades the noncancerous epithelial surface layers destructively, i.e., intraepithelial microinvasion (IEMI or superficial invasion).
(Fig. 13.4a, b)
Lesion (Fig. 13.4a, b)
V: Within this cancer, we see proliferation of microvessels with variable sizes, nonuniform morphology, asymmetrical distribution, and irregular arrangement. These microvessels form a dense tangle of open, closed, and irregularly branching loops. The vascular heterogeneity, with no two vessels with the same morphology or size, led to this being assessed as an IMVP.
S: We can see sections of MCE in the lesion margins with a curved to linear morphology. The MCE is lacking in continuity and consistent directionality, with variable IP size. In the central area, breaks and interruptions are seen in the MCE.
VS discordance: Dissociation is seen between the MCE and blood vessels, findings of VS discordance.
13.1.1.3 Histological Findings
13.1.2 Case 2: Typical IIc Type, IMVP Plus IMSP (Figs. 13.6–13.13)
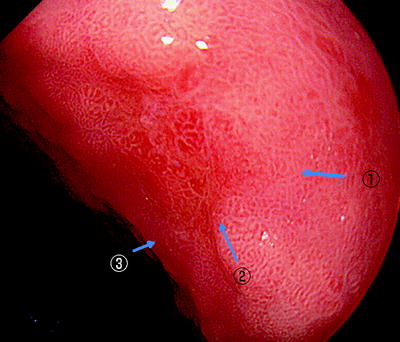
Fig. 13.6
On the posterior wall of the gastric body we can see a reddened irregular depressed lesion
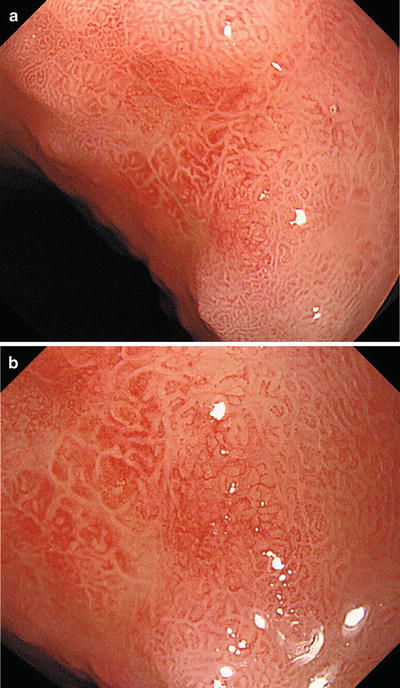
Fig. 13.7
(a, b) With the hood tip closely applied to the mucosa, if we increase the magnifying ratio slightly we can see the lesion margins clearly, but at this magnification we cannot discern the microvasculature
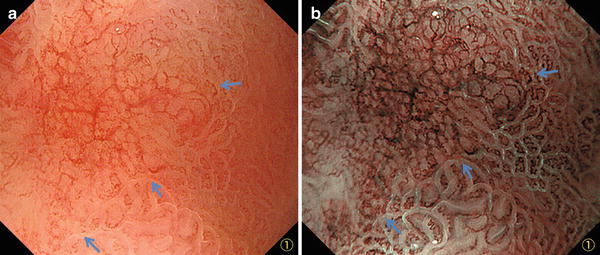
Fig. 13.8
(a, b) Marginal area corresponding to the area indicated by ① in Fig. 13.6 (explanation on the next page)
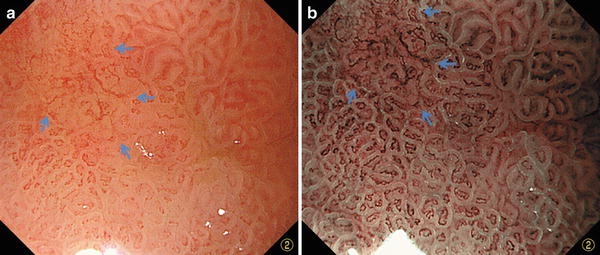
Fig. 13.9
(a, b) Marginal area corresponding to the area indicated by ② in Fig. 13.6 (explanation on the next page)
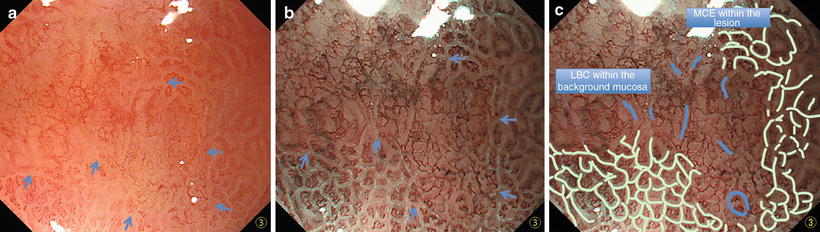
Fig. 13.10
(a–c) Marginal area corresponding to the area indicated by ③ in Fig. 13.6 (explanation on the next page)
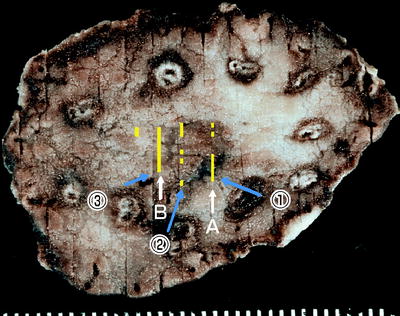
Fig. 13.11
ESD specimen (fixed in formalin). I have marked the areas corresponding to (1), (2) and (3) in Fig. 13.6
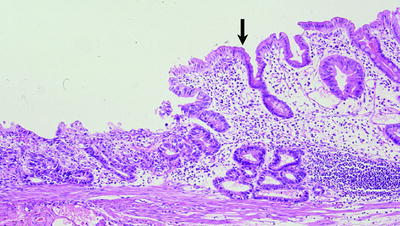
Fig. 13.12
Histological findings corresponding to the ME images in Fig. 13.8a, b, and section A in Fig. 13.11 The noncancerous background mucosa shows chronic gastritis associated with intestinal metaplasia. To the left of the marginal area (arrow), we can see a markedly depressed or excavated area with proliferation of small atypical glands with strong structural and cellular atypia. Since these glands are not aligned perpendicular to the mucosal surface, it is difficult to visualize the MCE morphology with a histological structure such as this
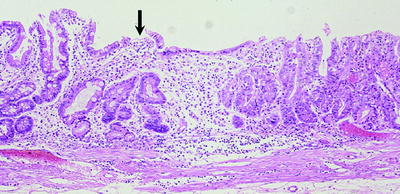
Fig. 13.13
Histological findings corresponding to the ME images in Fig. 13.10a, b, and section B in Fig. 13.11. The noncancerous background mucosa shows chronic atrophic gastritis associated with marked intestinal metaplasia. To the right of the marginal area (arrow), we can see cancerous tissue with a high glandular density. The glands in this area are long and tend to be aligned perpendicularly, so they meet the criteria for visualization of MCE
Posterior wall of the gastric body, 0 IIc type, differentiated type (well-differentiated adenocarcinoma), depth of invasion M, typical 0 IIc type on non-magnifying endoscopy, typical ME findings of EGC
13.1.2.1 Non-magnifying Endoscopy Findings
13.1.2.2 ME Findings (Low Magnification)
13.1.2.3 ME Findings (Maximal Magnifying Ratio)
Background mucosa
VS classification: regular MV pattern plus regular MS pattern
VS discordance: no
Marginal area
DL: present
IEMI: absent
Lesion
VS classification: irregular MV pattern plus irregular MS pattern
VS discordance: yes
Background mucosa (outside arrows in Figs. 13.8–13.10b)
V: Subepithelial capillaries with an open or closed loop morphology, symmetrical distribution and regular arrangement, form a regular honeycomb-like SECN.
S: Sections of MCE lined by LBCs (Fig. 13.10b, c) form regular polygonal IPs, resembling the gastric antral pattern.
VS discordance: Blood vessels are present in the IPs, so there is no VS discordance.
Marginal area (indicated by arrows in Figs. 13.8, 13.9, and 13.10)
We can see a clear DL corresponding to where the regular MV pattern plus regular MS pattern disappears. No findings consistent with IEMI are seen around the entire circumference of the DL.
Lesion (inside arrows in Figs. 13.8, 13.9, and 13.10)
V: The individual vessels show variability in size and morphology, forming irregular opened or closed loops. Most anastomoses are with other vessels, but the anastomoses are unequal and some are interrupted. The distribution is asymmetrical and the arrangement irregular.
S: We can just discern sections of curved MCE within the marginal area, but they are interrupted and irregular in direction.
VS discordance: No regularity can be seen in the MCE and MV arrangement or distribution, so there is VS discordance.
13.1.3 Case 3: Typical IIc Type, Irregular WOS (Figs. 13.14– 13.18)
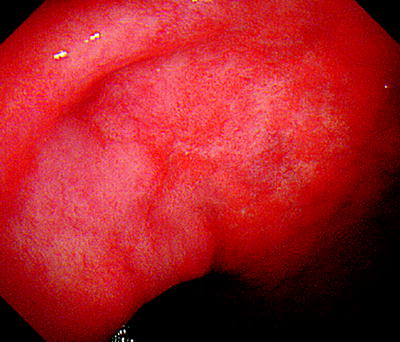
Fig. 13.14
On the posterior wall of the gastric antrum near the gastric angle we can see a slightly reddened flat area of mucosa with indistinct margins
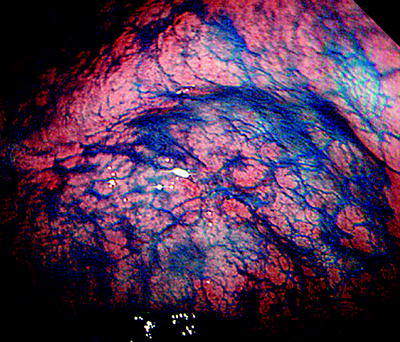
Fig. 13.15
With dye spraying, we can just discern a depressed lesion
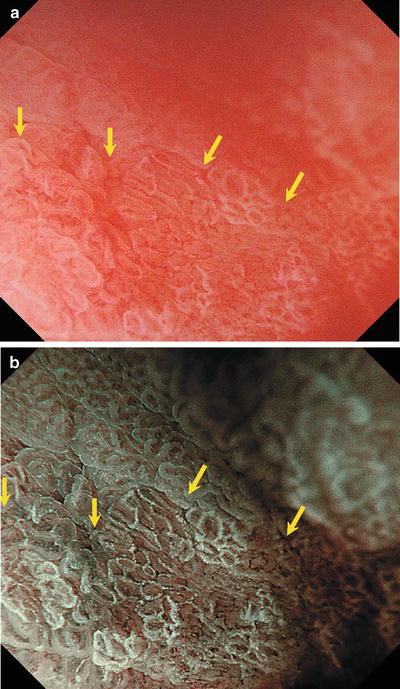
Fig. 13.16
(a, b) Marginal area (explanation on the next page)

Fig. 13.17
Lesion
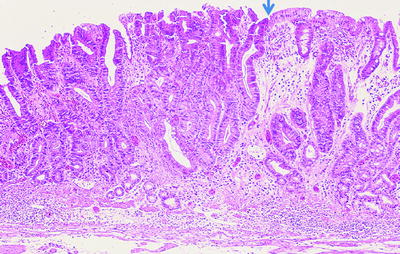
Fig. 13.18
Histological findings corresponding to the marginal area in Figs. 13.16a,b and 13.17. To the left of the marginal area (arrow), we can see a rather dense proliferation of neoplastic glands with marked cellular atypia. The nature of WOS is unclear, so we cannot explain the etiology of the ME findings
Posterior wall of the gastric antrum near the gastric angle, 0 IIc type, differentiated type (well-differentiated adenocarcinoma), depth of invasion M, typical 0 IIc type on non-magnifying endoscopy, typical ME findings of EGC.
13.1.3.2 ME Findings (Maximal Magnifying Ratio, Water Immersion Technique)
Background mucosa
VS classification: regular MV pattern plus regular MS pattern (LBC+)
VS discordance: no
Marginal area
DL: present
IEMI: absent
Lesion
VS classification: absent MV pattern plus irregular MS pattern (WOS+)
VS discordance: ND
Background mucosa (outside arrows in Fig. 13.16a, b)
V: Subepithelial capillaries with an open or loop morphology, symmetrical distribution and regular arrangement, form a regular honeycomb-like subepithelial capillary network (SECN).
S: MCE lined by LBCs forms regular oval IPs.
VS discordance: Capillaries are present in the IPs, so there is no VS discordance.
Marginal area (indicated by arrows in Fig. 13.16a, b)
We can see a clear DL corresponding to where the regular MV pattern plus regular MS pattern disappears. No IEMI findings are seen.
Lesion (inside arrows in Figs. 13.16a, b and 13.17)
V: The individual vessels predominantly form closed polygonal loops (Fig. 13.17), but the presence of WOS makes it difficult to clearly visualize and analyze the V component, so this was assessed as absent MV pattern.
S: Within the lesion we can see WOS in closed curves forming a reticular pattern. The WOS has a variable width and is discontinuous, leading to the assessment of an irregular MS pattern based on the WOS findings.
VS discordance: No MCE could be detected within the lesion, so this was assessed as not determined (ND).
13.1.3.3 Histological Findings
13.1.4 Case 4: Typical IIc Type, IEMI (Figs. 13.19–13.25)
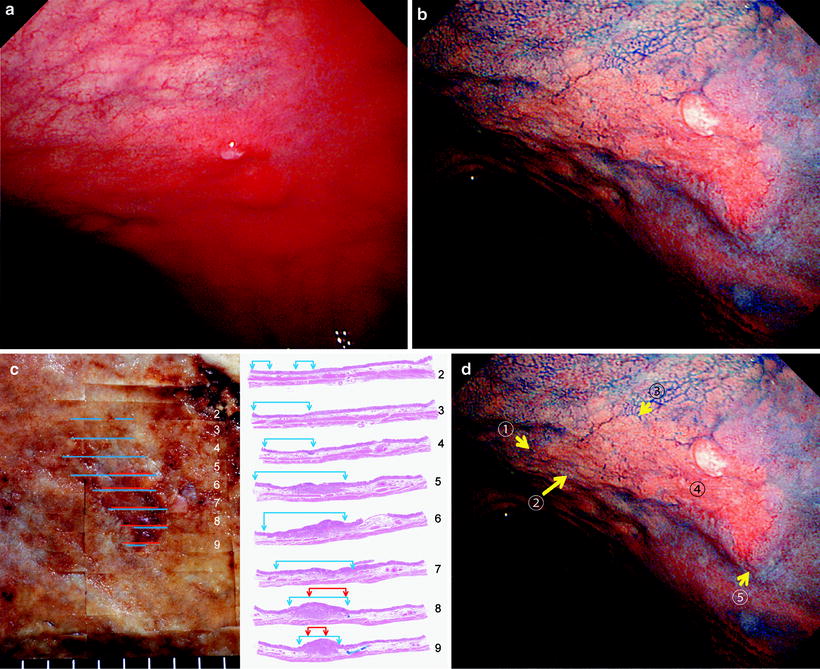
Fig. 13.19
(a–d) On the posterior wall of the upper gastric body we can see a depressed lesion with an irregular margin and invasion at the depressed margin. Dye spraying reveals the rise at the oral margin to be a sclerotic steep protrusion, findings consistent with penetration as far as the submucosa over the oral half of this depressed cancer. The surgically resected specimen shows invasion as far as the deep layers of the submucosa. (c) Blue lines: intramucosal cancer; red lines: submucosal invasion 13
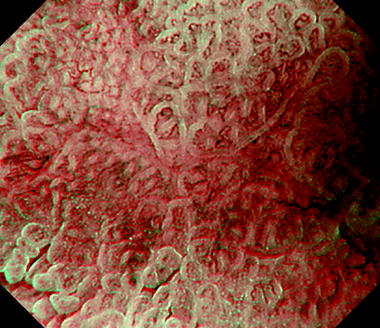
Fig. 13.20
Background mucosa

Fig. 13.21
(a–c) ME findings (IEMI: superficial invasion) of the area indicated by arrow 1) (marginal area) in Fig. 13.19d and the corresponding histological findings
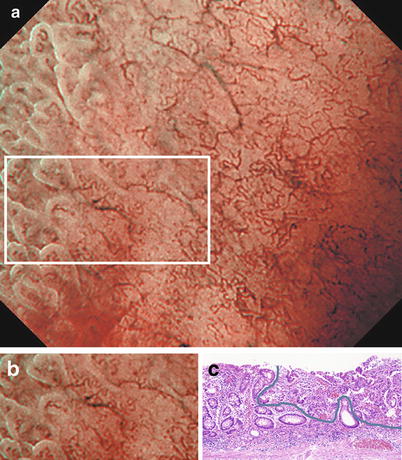
Fig. 13.22
(a–c) ME findings (IEMI: superficial invasion) of the area indicated by arrow 2) (marginal area) in Fig. 13.19d and the corresponding histological findings
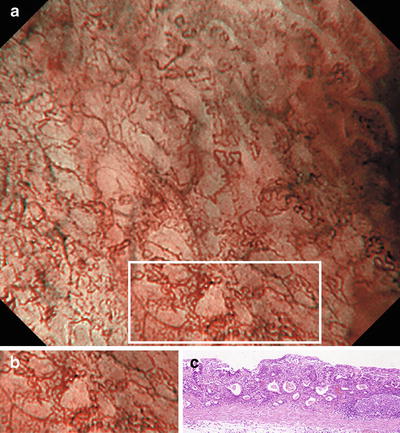
Fig. 13.23
(a–c) ME findings (dense close looped network) of the area indicated by arrow 3) (marginal area) in Fig. 13.19d and the corresponding histological findings
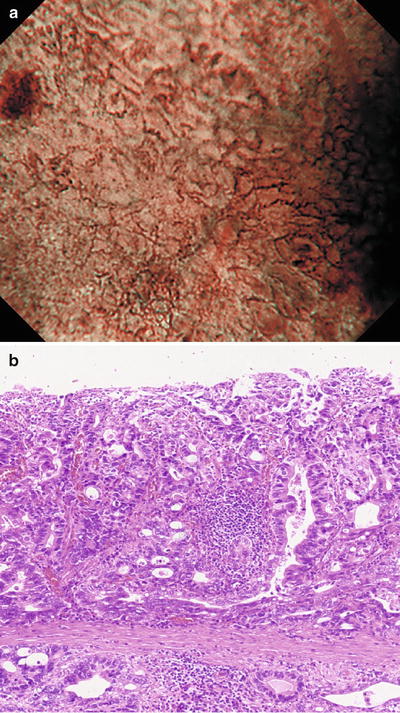
Fig. 13.24
(a, b) ME findings (multiple IMVPs) of the area indicated by arrow ③ (submucosal invasion by cancer) in Fig. 13.4d and the corresponding histological findings
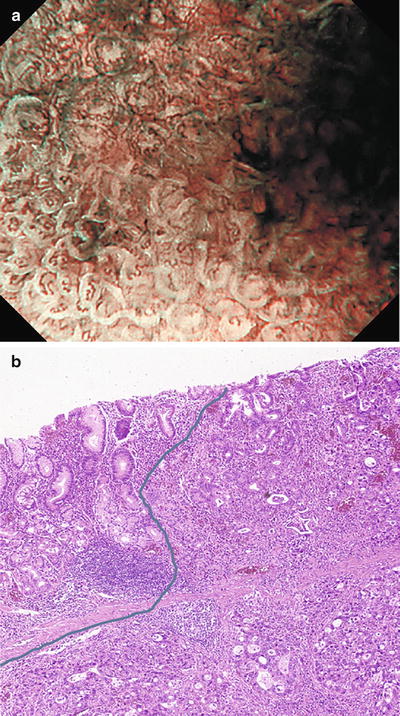
Fig. 13.25
(a, b) ME findings (IEMI: superficial invasion) of the area indicated by arrow ④ (marginal area) in Fig. 13.4d and the corresponding histological findings
Posterior wall of the upper gastric body, 0 IIc type, differentiated type (moderately to poorly differentiated adenocarcinoma), depth of invasion SM3, typical 0 IIc type on non-magnifying endoscopy, typical ME of EGC.
13.1.4.1 Non-magnifying Endoscopy Findings
13.1.4.2 ME Findings (Maximal Magnifying Ratio, Water Immersion Technique)
Background mucosa
VS classification: regular MV pattern plus regular MS pattern
VS discordance: no
Marginal area
DL: present
IEMI: present (superficial and subepithelial invasion)
Lesion
VS classification: irregular MV pattern plus absent MS pattern
VS discordance: not determined (ND)
Background mucosa (Fig. 13.20)
V: Small subepithelial capillaries have an open-looped or coil-shaped morphology. They stand alone, with a symmetrical distribution and regular arrangement.
S: Sections of MCE show a closed curved to crescentic structure, with a uniform width.
VS discordance: No dissociation of the V and S components is seen, so there is VS concordance (Figs. 13.21– 13.25).
Marginal area:
In the marginal area of the cancerous mucosa we can see a clear DL due to differences in the VS components between the cancerous and noncancerous mucosa. As shown in Figs. 13.21a and 13.22a, the cancer (IMVP) invades the IP epithelial surface of the noncancerous mucosa in an irregular and destructive manner. This is a marked intraepithelial microinvasion (IEMI). In cases with ME findings such as these, histologically the cancer is often invading the superficial layers of the noncancerous mucosa in a destructive manner (superficial invasion). On the other hand, in the marginal area with SM invasion in Fig. 13.25a, the MCE is preserved in the noncancerous mucosa, but we can see an irregular MV pattern underneath the epithelium. The histological findings reflect subepithelial tumor invasion (subepithelial invasion), as well as tumor in the deep mucosal layers compressing the epithelium, causing stretching and thinning.
Lesion (Figs. 13.21– 13.25)
V: In the area of IEMI in Figs. 13.21a–13.25a, we can see proliferation of microvessels with variable sizes, nonuniform morphology, asymmetrical distribution, and irregular arrangement. These microvessels form open, closed, and irregularly branching loops. Characteristic of the IMVP of this lesion is that the closed loops form a dense network with small individual loops. Another feature of this lesion is the absence of large irregularly branching vessels. In moderately differentiated adenocarcinomas, we sometimes observe a small dense closed looped network. In the area of subepithelial microinvasion in Fig. 13.24a, the vessel density of the IMVP is increased three dimensionally. In fact, we can see a complex structure with a brown subepithelial IMVP and a somewhat deeper cyan-colored IMVP, in other words multilayered IMVPs.
S: We can see no MCE or other mucosal microsurface structures, so this is an absent MV pattern. Histologically, this tumor comprises small shallow neoplastic glands, seen as an absent MV pattern.
VS discordance: No MCE could be detected, so VS concordance could not be assessed. It is therefore not determined (ND).
13.1.5 Case 5: Small IIc Type, MCE Elements (Figs. 13.26–13.35)
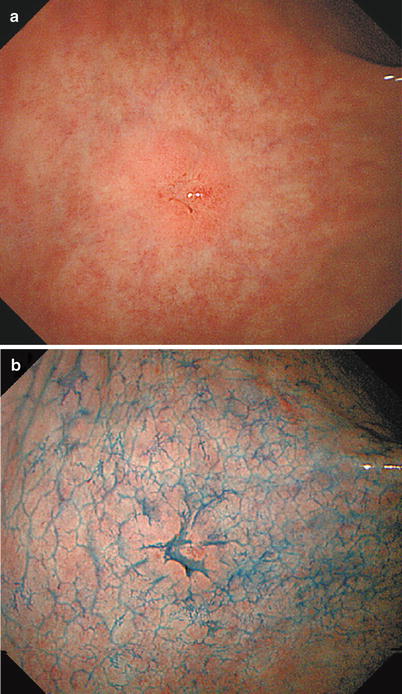
Fig. 13.26
(a, b) On the anterior wall of the gastric antrum, we can see a small depressed lesion with an irregular margin slightly raised on the inside. There are also spiny depressions
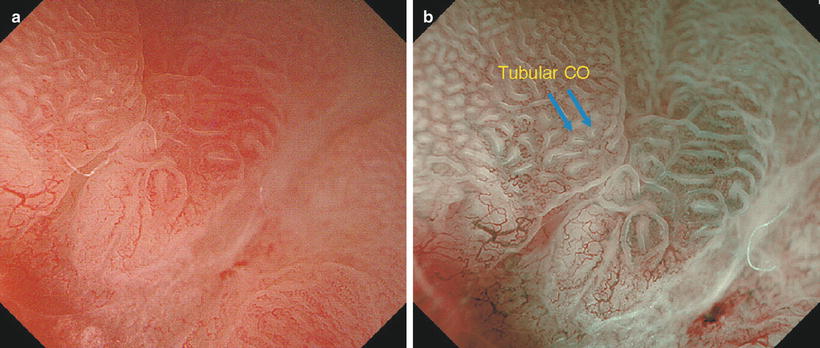
Fig. 13.27
(a, b) ME findings (explanation on the next page)
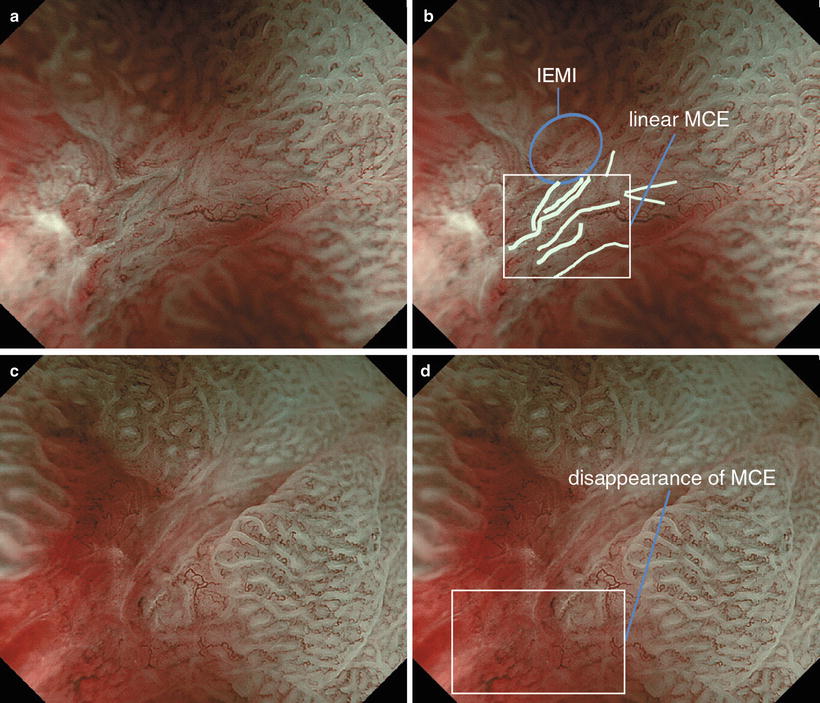
Fig. 13.28
(a–d) ME findings (explanation on the next page)
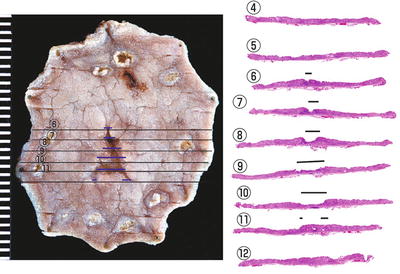
Fig. 13.29
Mapping of the ESD specimen (fixed in formalin) and the corresponding loupe images. The upper half of the depressed area on the resected specimen corresponds to the grooved depression seen endoscopically
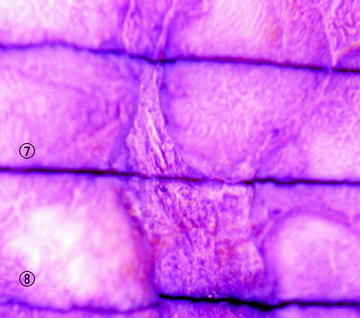
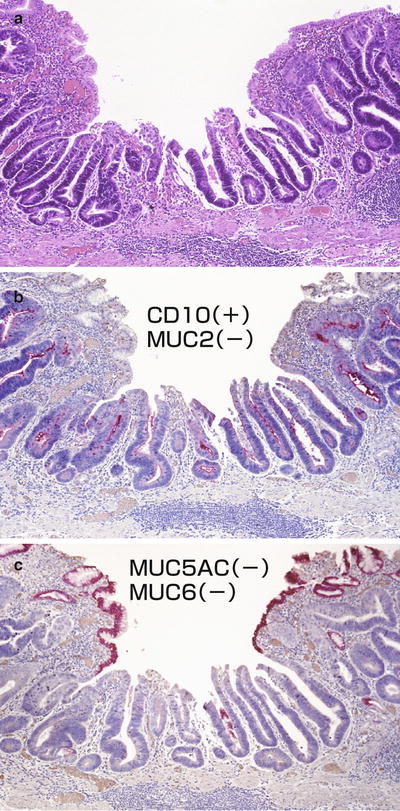
Fig. 13.31
(a) Section ⑦ under high magnification (25×). Although the glands do not run perfectly perpendicularly, we can see the openings of relatively large neoplastic glands of simple non-branched tubular form (b). Anti-CD 10 immune staining was positive on the luminal surface of the neoplastic glands. Although not shown here, MUC2 mucin staining was negative (c). MUC5AC mucin staining was positive in the noncancerous foveolar epithelium mucin, but negative in the tumor cell mucin. Although not shown here, MUC6 mucin staining was also negative. Accordingly, we concluded that this gastric cancer has the small intestinal phenotype
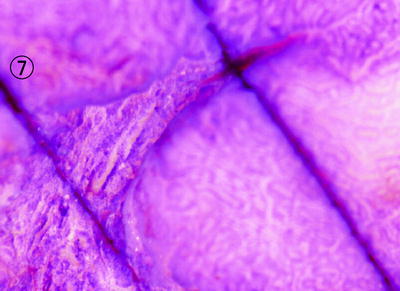
Fig. 13.32
Carazzi’s hematoxylin-stained stereoscopic microscopic findings
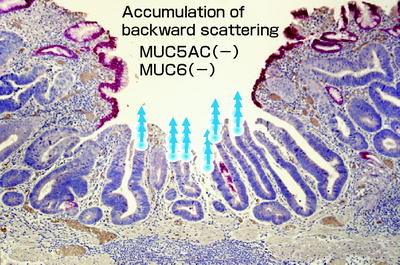
Fig. 13.33
If we project light into the neoplastic glands running perpendicular to the surface in Fig. 13.31c (MUC5AC mucin staining), continuous backward scattering accumulates within the perpendicularly aligned cells, as indicated by the arrows
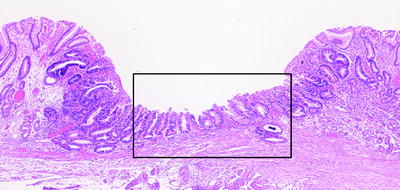
Fig. 13.34
Low magnification (10×) image of the histological findings of section (8)
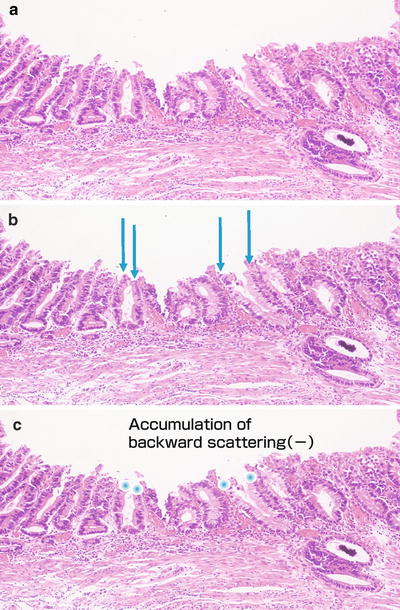
Fig. 13.35
(a–c) High magnification (25×) images. Projected light (arrows) does not undergo continuous backward scattering
Anterior wall of the gastric antrum, small 0 IIc type, 8 mm in diameter, differentiated type (well-differentiated adenocarcinoma), depth of invasion M, typical 0 IIc type on non-magnifying endoscopy, typical ME findings.
13.1.5.1 Non-magnifying Endoscopy Findings
13.1.5.2 ME Findings (Maximal Magnifying Ratio, Water Immersion Technique)
Background mucosa
VS classification: regular MV pattern plus regular MS pattern
VS discordance: no
Marginal area
DL: present
IEMI: present
Lesion
VS classification: irregular MV pattern plus irregular MS pattern
VS discordance: yes
Background mucosa (Figs. 13.27 and 13.28)
V: The individual vessels are predominantly small coil-shaped subepithelial capillaries characteristic of the gastric antrum. They stand alone, with a symmetrical distribution and regular arrangement.
S: The sections of MCE show a curved or linear structure, with a uniform width. They are arranged in orderly lines, with a symmetrical distribution. In just one area, we can see some tubular COs (Fig. 13.27b).
VS discordance: No dissociation of the V and S components is seen, so there is VS concordance.
Marginal area (Figs. 13.27 and 13.28)
In the marginal area of the cancerous mucosa, we can see a clear DL corresponding to where the V and S components change. As shown in Fig. 13.27a, b, a cancerous IMVP can be seen beneath the IP epithelium in cancerous mucosa. These are the findings of IEMI (subepithelial invasion).
Lesion (Figs. 13.27 and 13.28)
V: The individual vessels are irregularly branching, open-looped, or variably sized closed looped vessels. Their morphologies and sizes show considerable heterogeneity and irregularity. The distribution is asymmetrical and the arrangement irregular. These findings correspond to the typical IMVP for a differentiated carcinoma.
S: The sections of MCE in the groove-like marginal depressions are belt-shaped, with five or six wide strips extending a considerable distance (Fig. 13.28a, b). MCE has disappeared in the depressed central area (Fig. 13.28c, d). Overall, the paths and morphologies of the sections of MCE are irregular, and this is an irregular MS pattern.
VS discordance: No consistent regularity can be seen in the V and S components, so this was assessed as VS discordance. A feature of this lesion is the presence of irregularly branching large microvessels in the IPs.
13.1.5.3 Comparison of Histological and ME Findings
With this small lesion, using the groove-like marginal depressions as a marker, we can readily compare the resected specimen and the ME findings. Here I will give a simple explanation of the VS components as visualized using ME, and the histological findings, particularly of the groove-like depressions (Figs. 13.29–13.33).
I presented the above immunohistochemical-stained specimens for the following two reasons: (1) to enable a discussion about why LBCs are not visualized using M-NBI on the margins of the CD 10-positive neoplastic glandular epithelium and (2) it is easy to distinguish between tumor and nontumor epithelium, as the tumor stains negatively for MUC5AC and the nontumor foveolar epithelium stains positively for MUC5AC.
1.
Conditions for visualization of LBCs (Fig. 13.28a)
Figure 13.28a If we reexamine the M-NBI images of the groove-like area of the depressed margin, with an understanding of the above histological findings in mind, we can just discern LBC-like borders on the margins of the belt-like sections of MCE, although they are indistinct. A possible reason may be that, as shown in Fig. 13.31b, the neoplastic glandular epithelium stains positively for CD 10, and a brush border is present, but it is not aligned in parallel along the direction of the incoming light. In other words, the brush border is not aligned in a uniform direction and is therefore not recognizable as an LBC. Incidentally, only the brush border on the MCE that is parallel to the incoming light is visualized as an LBC. Even if a brush border is present on the IP surface epithelium, it is not visualized as an LBC using ME. We can surmise that the condition that must be met for a brush border to be visualized as an LBC is that the brush border is aligned in a direction parallel to the path of the incoming light.
2.
Figure. 13.32. This figure shows a stereoscopic microscopic image in the same alignment as Fig. 13.28a. Between the belt-shaped structures of the sections of MCE, we can definitely discern some groove-shaped COs.
Figure 13.33. This figure shows MUC5AC staining, with nonneoplastic crypt epithelium staining red. There are four neoplastic glands opening onto the surface. Moreover, there are around six columns of MCE aligned perpendicularly with a uniform width, so as I explained in Chap. 8, we can only visualize around six columns of MCE through backward scattering of projected light. This is the reason we can observe five or six sections of belt-shaped MCE within the groove-like depression on the tumor margin.
3.
IEMI
As shown in Fig. 13.31c, tumor invading underneath the normal epithelium possesses a stroma. An IMVP can be detected using ME, and the noncancerous microsurface structure is preserved. This particular example of IEMI shows subepithelial invasion, with an IMVP continuous with the tumor seen under the non-neoplastic epithelium.
4.
See Fig. 13.28d Disappearance of MCE.
Here we review Fig. 13.28d again, with an area with an absent MS pattern, characterized by disappearance of MCE and a flat appearance with no mucosal microsurface structure. In the stereoscopic microscopic image in Fig. 13.30, corresponding to the depressed area in Sect. ⑧, this area is enclosed by a fine MCE. Although small, we can discern COs an irregular tubular morphology. In the low magnification (10×) image of the histological findings of Sect. ⑧ (Fig. 13.34) we can also see small, densely packed, malignant glands with a tubular structure. The reason this MCE cannot be visualized using ME is unclear, but we can see that in comparison to the malignant glands in Fig. 13.31a the crypts are small and shallow and the MCE is oriented obliquely, as shown in the high magnification (25×) image (Fig. 13.35a). Accordingly, it may be that backward scattering does not accumulate uniformly within the epithelium, so it is not visualized as MCE, causing an absent MS pattern. The degree of scattering is also thought to vary according to the nature of the epithelial cells, so the real reason why neoplastic MCE lining small shallow crypts with an oblique orientation is not visualized is a question yet to be answered. In any case, I would like to emphasize that the presence of tubular adenocarcinomatous tissue even with an absent MS pattern (i.e., no MCE, WOS, or LBC, markers of the mucosal microsurface structure, can be discerned) is an important presupposition in the interpretation of ME findings of glandular epithelium. The reason I set the diagnostic criteria for carcinoma as an irregular MV pattern or an irregular MS pattern is that some lesions, and not uncommonly differentiated carcinomas, yield findings with ME with WLI or NBI of an absent MS pattern, if in vivo staining is not performed.
13.1.6 Case 6: Small IIc Type, Irregular WOS (Figs. 13.36–13.39)
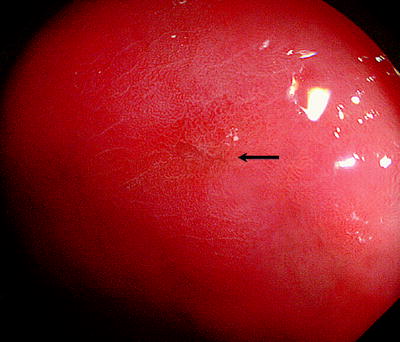
Fig. 13.36
On the posterior wall of the gastric antrum near the gastric angle, we can see a small pale depressed lesion (arrow). We cannot identify any spiny depressions or irregular margins characteristic of malignancy, so this lesion cannot be diagnosed as a cancer using non-magnifying endoscopy
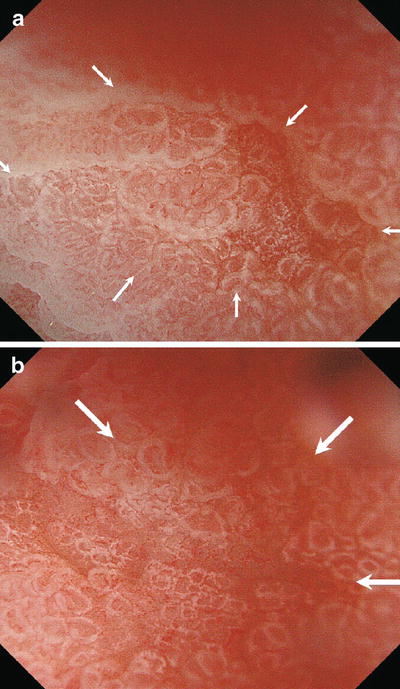
Fig. 13.37
(a, b) Marginal area
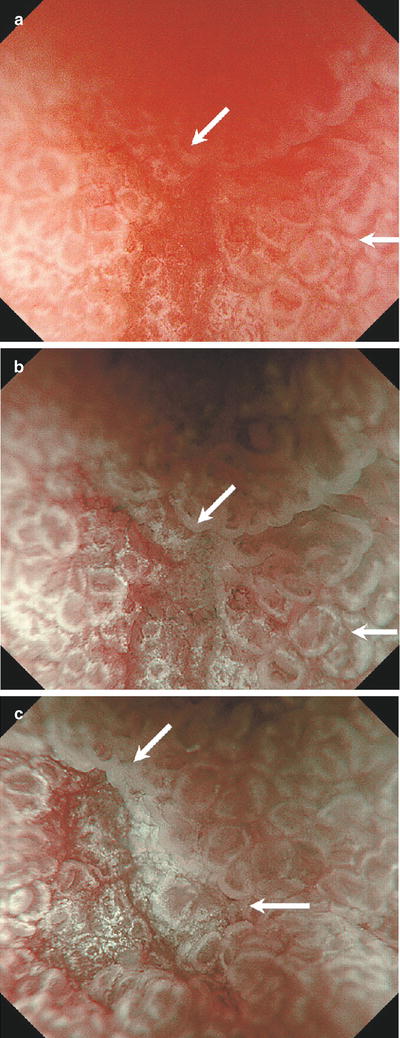
Fig. 13.38
(a–c) Marginal area
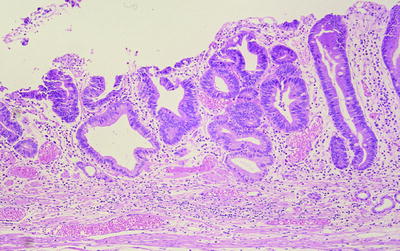
Fig. 13.39
This is a well-differentiated adenocarcinoma. The nature of WOS is unclear, so we cannot make direct comparisons between the histological findings and ME images. This remains a challenge for the future. The background mucosa shows atrophic gastritis associated with intestinal metaplasia
Posterior wall of the gastric antrum near the gastric angle, minute 0 IIc type, 4 mm in diameter, differentiated type (well-differentiated adenocarcinoma), depth of invasion M, atypical 0 IIc type on non-magnifying endoscopy, typical ME findings of EGC.
13.1.6.1 Non-magnifying Endoscopy Findings
13.1.6.2 ME Findings (Maximal Magnifying Ratio, Water Immersion Technique)
Background mucosa
VS classification: absent MV pattern plus regular MS pattern (WOS+)
VS discordance: no
Marginal area
DL: present
IEMI: absent
Lesion
VS classification: absent MV pattern plus irregular MS pattern (WOS+)
VS discordance: yes
Background mucosa (outside arrows in Figs. 13.37 and 13.38)
V: The individual vessels are predominantly small coil-shaped subepithelial capillaries characteristic of the gastric antrum. In some areas they can be seen to stand alone, with a symmetrical distribution and regular arrangement, but due to the presence of WOS thought to be associated with intestinal metaplasia, we cannot see any detail, so this was assessed as an absent MV pattern.
S: The sections of MCE show a curved or linear structure, with a uniform width. They are arranged in orderly lines, with a symmetrical distribution.
VS discordance: No dissociation of the V and S components is seen, so there is no VS discordance. There are one or two capillary loops in each IP.
Marginal area (indicated by arrows in Figs. 13.37 and 13.38)
We can see a DL corresponding to the changes in the mucosal microsurface structure given below.
Lesion (inside arrows in Figs. 13.37 and 13.38)
V: As shown in Fig. 13.37a, M-WLI revealed WOS, making it impossible to analyze the subepithelial microvascular pattern, so this is an absent MV pattern. Closely applying the hood tip to the mucosa and overstretching the depressed area, we can just discern some microvessels in the base of the depression, but we cannot assess their morphology.
S: If we focus on the WOS in Fig. 13.38c, it has a speckled pattern, with an asymmetrical distribution and irregular arrangement. This was assessed as an irregular MS pattern based on the presence of irregular WOS.
VS discordance: Dissociation between the WOS distribution and the distribution of the microvessels visible in some areas led to the assessment of VS discordance.
13.1.6.3 Histological Findings
13.1.7 Case 7: Typical IIc Type, RMVP Plus RMSP (Figs. 13.40–13.46)
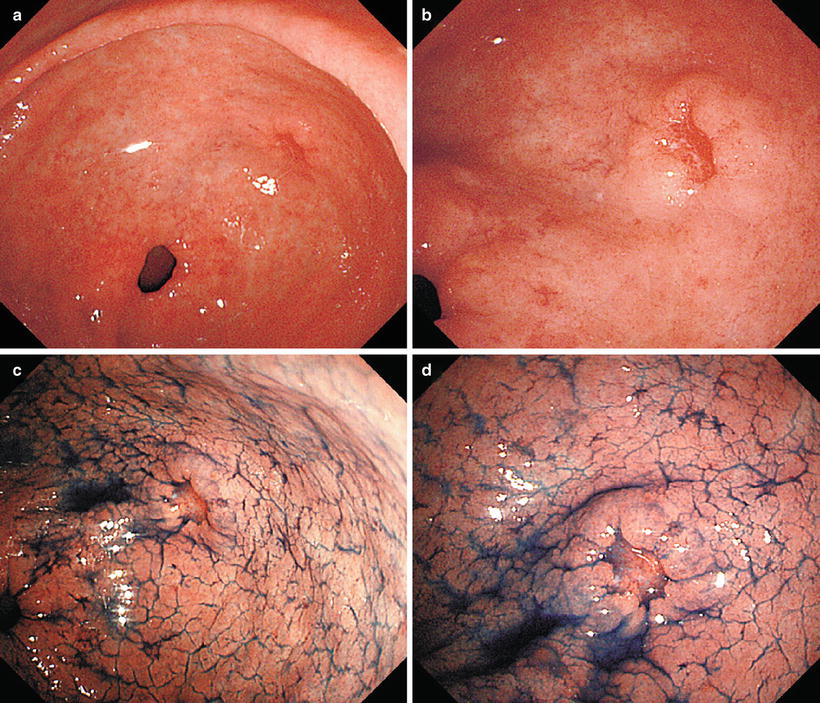
Fig. 13.40
(a–d) On the posterior wall of the gastric antrum, we can see a reddened depressed lesion with an irregular margin slightly raised on the inside
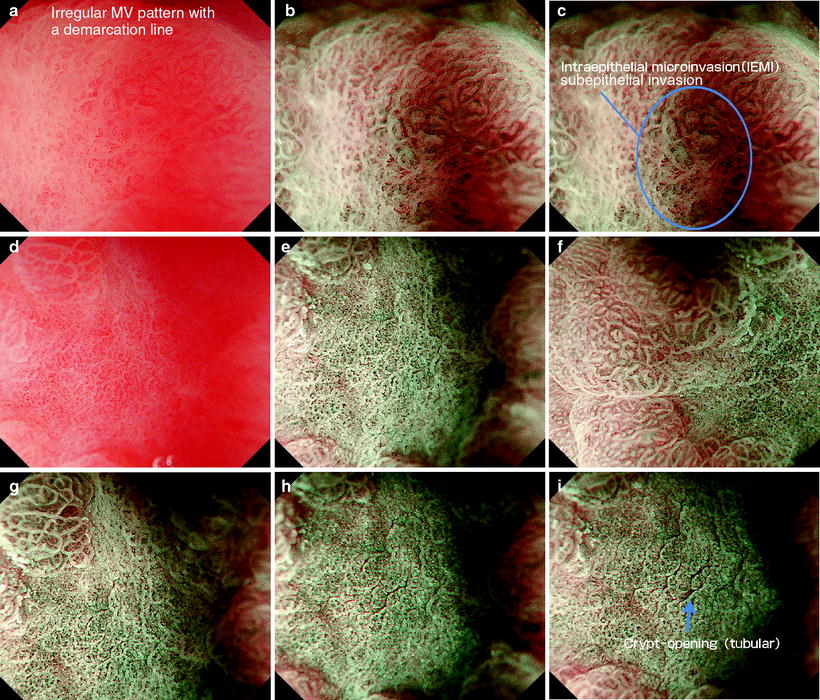
Fig. 13.41
(a–c) Marginal area IEMI. (d–f) RMVP plus RMSP with a DL (g–i) Visualization of COs using the water immersion technique. With the black hood closely applied to the lesion, instillation of water causes the CO spaces to open due to the water pressure, allowing visualization of the groove-like indentations
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







