Many men do not take recommended measures to screen for prostate cancer. Additionally, insurance companies have not always reimbursed for cancer screenings. This article highlights the Washington State Urology Society’s efforts at improving patient outcomes through legislatively mandated cancer screenings.
How many men have urologists seen who present for evaluation of concerns regarding erectile dysfunction, prostate cancer, vasectomy consultation or evaluation of genital pains, who have no contact with a primary care physician? These men are not referred and are unaware of potential health issues either associated with the condition for which they are seeking care, or they are related to a positive family history for a major disease entity.
Additionally how many referred patients are urologists asked to see for whom the patients’ referring physician is unaware of the systemic multiorgan implications of the urological issue being addressed? In both situations the evaluating urologist may have the opportunity to significantly impact the patient’s wellbeing. Clearly the male patient who is advised that his difficulties with sexual health lie in multiple system dysfunction is provided with evaluation and treatment that not only address erection issues but may be lifesaving as well. How many patients have returned after such an encounter to say thank you, commenting that had they not been referred on for medical care, would have most likely suffered a stroke or myocardial infarction and considered the identification of underlying obesity, diabetes, hypertension, and coronary artery disease a lifesaving intervention? Similar is the patient who responded to the suggestion that he have a colonoscopy, and was found to have an early and curable stage of colon cancer.
These are not unique stories to those who practice, yet a pattern of male patients at risk due to lack of entry into the health care system has repeatedly presented itself, and still occurs with regularity.
To improve opportunities for men to recognize the importance of a timely entry into the health care system, The Washington State Urology Society embarked upon a campaign to educate men and their families. Men were felt to be lacking the necessary information in how to take care of themselves, and correction of this knowledge deficit was considered a reasonable remedy. In 1994, The Men’s Health Seminar series was developed, and the first seminar was held in the spring of 1995.
A well organized state urology society
Integral to the ability to initiate and carry forth a campaign on male health was a well organized and supported state society. The Washington State Urology Society was established in 1984, with a committed membership and board of directors. The society also benefited from the fact that its leadership included urologists who were active within the American Urological Association, The American Association of Clinical Urologists, and the American Board of Urology.
Most importantly, the leadership of the society was welcoming and nurturing to those newly minted from residency training. This tradition of engagement carries on today and provides for a continued integration of efforts both from rural and suburban, large and small practices, and academic and nonacademic practices.
The Men’s Health Seminar Series was thus coordinated throughout the state, with urologists and other medical specialties. A typical presentation would include an introduction by a primary care physician who served as moderator and spoke about how to get the most out of the primary care visit.
Information on diet, cardiac disease/hypertension, colorectal cancer, gastroesophageal reflux disease (GERD), skin cancer detection and prevention, and what men should know about hair loss and baldness was also presented. Urological topics included prostate cancer detection and treatment, benign prostate disease, and impotence. The urological presentations were from various institutions and practices. The benefit to the attendees was a coordinated effort to encourage men to assume a more active role in health care and prevention. The benefit to urology and other specialties was the opportunity to educate the public regarding what strategies and investigations specialty physicians felt were important to the health maintenance of the population, rather than have legislators or other nonphysician groups provide less evidence-based data.
The timing was important, as the national health care climate during that time period was much like the current agenda. Of concern for those in active practice were issues regarding access to specialty care and restrictions on ability to practice. The format of the seminars allowed the public to hear directly from care providers about current care recommendations and what was felt to be current practice standards.
The limiting factors were attendance, which was limited to auditorium capacity, and the fact that most attendees were seniors. The seniors gave tremendous feedback regarding the content of the seminars. One recurring theme was that the seniors wished they had the opportunity to have received the information decades earlier. The benefit from the information provided to the population was felt to be more relevant to the younger man.
Reviewing this information with the dilemma of space constraints and difficulty in reaching younger men, who would be more likely to be at work during the day, or attending the needs of family in the evening, it became clear a different approach was needed. Perhaps the information from the seminars could be developed into a printable guide. Researching available materials regarding men’s health yielded surprisingly few satisfactory materials. A book on men’s health was available through the American Medical Association (AMA); however, it was very comprehensive, and was a difficult quick read. It appeared to be the type of book that would appeal to an individual who was seeking in-depth information. It was not generally something an average young man would be able to obtain directions for health maintenance from at a glance.
Many other materials suffered from the opposite issues. They contained too little. Pamphlets that suggested a man should get a colon check, watch his weight, eat well, and manage blood pressure, contained very little specific information regarding how to and when undertake care. Additional search of the literature under male health yielded information on sexually transmitted disease (STD) prevention or health-specific recommendations regarding sexual health. The report of the Commonwealth Fund was one of the few publications to report on male health disparity. Additionally, articles by Will Courtney discussed the male tendency to defer care and intervention due to male enculturation. It was clear that more was needed in terms of information on general health maintenance for men.
The Washington State Urology Society executive committee agreed to move ahead with the development of its own booklet. The executive committee felt that the society could provide the necessary information for what men would require, or need to learn and do to enter into appropriate health care maintenance. A Guide to Men’s Health was developed as an appropriate tool, with sufficient information for the public to realize the care associated with and health strategies involved in male health maintenance.
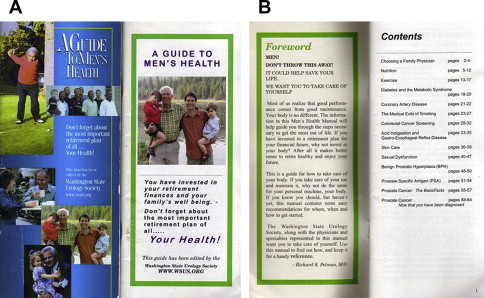
Authors were sought from the group of presenting physicians of the seminar series. Each presenter was tasked with writing up his or her presentation for a printed format. The goal was to provide sufficient information for the population to understand the why, what, and when of initiating health care. The idea of a male health maintenance manual synched nicely with what was felt to be adequate information without being overly burdensome to read. The Guide to Men’s Health ( Fig. 1 ) was printed through an unrestricted educational grant from Bayer Pharmaceuticals (Wayne, NJ,USA) in 2003.
Distribution of the printed guide was undertaken with the cooperation of human resource directors of various national and international corporations based in Washington State.
During one such discussion the question was raised: “How do we know a guy who has read it will make an appointment?” Clearly knowledge deficit was only partially responsible for the deficit in male attendance to care. To better answer that question, a collaboration with the Department of Anthropology at the University of Washington was undertaken to further elucidate male health. The pilot study designed to help in developing further data in this regard was by Dr Katherine O’Connor and her team.
Distribution of the printed guide certainly allowed for a greater number of men to access information; however, the opportunity to engage the male population required even a broader reach. Fortunately, the Internet allowed for electronic posting of the guide and the placement of not only the printed Guide to Men’s Health, but the posting of video chapters as well. Both versions, as well a Guide to Women’s Health, are available at the Web site for the Washington State Urology Society, www.wsus.org .
The video chapters have been well received and have allowed for far greater access to information on male health than the society’s first seminars.
Advocacy creates more advocacy
In the Washington State Urology Society’s efforts to promote the guide and the men’s health agenda, opportunities to meet and engage various other organizations presented collaborations that became beneficial to male health. The experience of promoting the Guide to Men’s Health along with the Washington State Urology Society’s male health campaign brought together groups that had previously been unaware of each other’s efforts. These local organization members were happy to see urologists active in public advocacy on behalf of men. The collaboration with physician champions was helpful in uniting an effort toward promoting the common goal of improved communication toward male health awareness and the importance of pursuing legislative remedies to protect a man’s ability to receive appropriate testing as recommended by his health care practitioner. Prostate-specific antigen (PSA) was not routinely being covered by all insurance plans, and in some instances letters from the treating health care professional were required along with supporting documentation with denial still occurring after review.
The relationships developed through the combined advocacy of groups coming together, along with unified acceptance by all parties that prostate cancer detection should be available to all men in Washington State led to a successful legislative campaign. The legislative campaign in the Washington capitol, Olympia, would not have been successful without someone to coordinate the effort. Fortunately, the Washington State Urology Society benefited from a well organized, energetic, and knowledgeable executive director, Debi Johnson, who led the initiative through all the steps and hearings necessary for passage. The process from proposed legislation to passage would not have occurred if Johnson and other committed individuals had not personally guided the bill through the many stages to passage. The ability to band groups together with a common goal allowed legislators to see and hear from not only physician advocates but public advocates as well.
The successful passage of a mandate such as SB 6188 (2006 prostate cancer screening) during a short legislative session in one of the most highly mandated states in the country did not happen overnight. The process took approximately 18 months to complete.
Step 1
Step 1 was identification of an advocacy need that could be translated into a parity bill with a minimal fiscal note. The coverage for prostate cancer screening varied among insurance plans at the time and often involved significant time spent by medical practices to verify benefits for their patients. High-risk patients were receiving their first prostate cancer screen at age 50 and were sometimes diagnosed with late-state disease. This was resulting in increased mortality rates and higher health care costs related to treating these patients. This was frustrating to both the prostate cancer survivor community as well as urologists, knowing prostate cancer is often treatable if diagnosed early. After becoming more informed about the current mammography legislation, Deborah A. Johnson decided there was a need for parity legislation to bring about similar access to prostate cancer screening as there was for breast cancer screening.
Step 2
Through informal interviews with urologists and prostate cancer survivors, it was decided the legislation had to address four critical elements. First, the decision as to whether to screen someone for prostate cancer would no longer be the decision of health insurers. The decision needed to be put back in the hands of medical professionals. Second, the timing of prostate cancer screenings needed to be coordinated by the medical professionals. Third, there needed to be an increased emphasis on prostate cancer awareness for the high-risk populations. Finally, the legislation had to be timeless and nonspecific to a particular screening method, since there were controversies over best practices.
Step 3
Create a public forum to raise awareness for the advocacy need that incorporated all of the key stakeholders and legislative influencers. These included physicians, leaders of primary patient advocacy groups, local television celebrity, chairperson of the Senate Healthcare Committee, longstanding member on the Senate Health and Long-term Care Committee. Bipartisanship was the key to having any legislative movement on this effort.
Funding for the public forum and patient outreach event was provided by TAP Pharmaceuticals (now known as Abbott Laboratories; North Chicago, IL, USA). The solicitation for the grant funding started in the fall of 2004, when the strategic vision was created. On July 23, 2005, a program called Safe at Home was added to the Regional Softball USA Tournament. Men aged 50 years and older from around the state of Washington and across the country engaged in tournament play and were given the opportunity for a free screening and participation in prostate cancer awareness education. Screenings challenges were set up between the teams regarding “knowing their scores.” Key players in the education forum were:
Physicians (Chris Porter, MD, Washington State Urology Society Men’s Health Committee member and cochairman of Virginia Mason Medical Center’s Urologic Oncology Division)
“Common Urologic Diseases Every Man should know” –Title of the Education Forum given by Dr Chris Porter.
Patients (including high-risk populations)
President, Seattle Chapter US Too International
Treasurer, US Too International Corporate
Chair, Prostate Cancer (PCa) Task Force of the Washington CARES about Cancer Partnership
President, Man-to-Man Tacoma Chapter
African American Pediatrician PCa survivor
Local television celebrity and PCa survivor
Founder, Safe-At-Home: Prostate Cancer Awareness Network
Legislators on the Senate Health and Long-term Care Committee participated in the town hall meeting on men’s health including prostate cancer, which was incorporated into the Safe-At-Home project. (Senator Karen Keiser [D] and Senator Stephen Johnson [R]). It was important to have them at the town hall and have it televised on the local Public Access Network. The goal for the town hall meeting was to capture on film the commitment by legislators to do something in the next legislative session concerning men’s health and prostate cancer. The authors were successful in getting a bipartisan commitment to address the issue in the 2006 legislative session.
Step 4
Capture the dialog
The use of a regional nonprofit digital media company and connections with the Public Access Network allowed all of the lectures and panel discussions during the Safe At Home town hall meeting to be captured digitally. Three- to 5-minute edits were created to enforce legislative commitments made during the educational forum. The prostate cancer screening material presented at the forum was edited and streamlined for a comprehensive reference DVD for the senators.
Step 5
Step 5 involves identifying mentors for the legislative process and coordinating partners.
The American Association for Clinical Urologists (AACU) was used as a mentor in the general legislative process. The AACU provided written testimonials that the Washington State Urology Society executive director submitted during legislative hearings. The Washington State Medical Association’s (WSMA) director of public policy assisted with the nuances of the Washington State legislature and provided guidance for overcoming potential objections with specific legislators. Although the WSMA could not support the bill because of its policy concerning mandates, the Washington State Urology Society coordinated with members not to publicly state they were against the bill.
The Washington State Urology Society executive director (independent association management contractor and business development consultant) conducted joint strategy sessions with both the TAP Pharmaceuticals and the National Prostate Cancer Coalition’s government affairs representatives. The government affairs representative for TAP Pharmaceuticals provided local government insight concerning key legislative players that expedited the process. He lobbied his connections in the state senate and house. His past personal experience working in the Washington State Legislature was helpful. He worked closely with the Washington Legislative Committee staffers to get the behind the scene communications on the status of the bill and made the Washington State Urology Society aware of Novartis Pharma involvement, which increased exposure for the bill.
The National Prostate Cancer Coalition provided additional written testimonials and press releases. In-person testimonies at the legislative hearing were provided by:
US Too International
Man-To-Man
Prostate Cancer Awareness Network
Virginia Mason Medical Center urologist (also provided awareness pins and was instrumental on conducting the free screenings during the Safe At Home event July 2005)
Executive director for the Washington State Urology Society (also purchased pink/blue family pins to reiterate the parity issue surrounding the bill)
Prostate Net
Washington State Prostate Cancer Coalition
American Cancer Society (also provided PCa awareness pins)
Comprehensive Cancer Control Partnership (provided its endorsement).
Step 6
Step 6 involved drafting proposed legislation that met the criteria.
The authors networked with multiple national organizations to identify the best player to assist with drafting of the legislation. It was important to incorporate a national organization that did not appear to have a perceived set agenda (eg, The American Urological Association [AUA] would have a tendency to look like the legislation had a financial benefit to physicians). The National Prostate Cancer Coalition (now known as “ZERO—The Project to End Prostate Cancer”) was chosen to be the best partner for this aspect of the strategy.
Step 7
Step 7 involved identifying legislative champions.
Follow-up to the Safe At Home town hall event took place in the fall of 2005. Both Senators Keiser and Johnson were contacted to sponsor the drafted bill. The senators agreed that Senator Johnson would be the best to sponsor it, since Senator Keiser was the chairwoman of the Health and Long-term Care Committee. The Washington State Urology Society cross-referenced recent state legislative speakers for their annual meetings to identify additional champions for the bill. (Linda Evans Parlette (R) and Mary Skinner (R) [diseased as of February 5, 2009]). Additional champions were identified by cross-referencing the Washington State Urological Society/AACU members with legislators sitting on key committees involved with the passage of the bill.
Decision influencers in the legislative process include
Introduce legislation—Senator Johnson
Schedule bill on Senate Health Care Committee agenda and put it up for executive session—Senator Keiser, Chairwoman of Senate Healthcare
Pull bill out of Senate Rules Committee—Senator Johnson
Place it on the Senate Floor for vote—Senator Tracey Eide (D), Senate Floor Majority
Schedule bill on House Healthcare Committee agenda and put it up for executive session—Representative Eileen Cody (D), chairwoman of House Healthcare
Appropriations hearing agenda and passage—no champion was identified; solicited support from all members of Appropriations committee
Pull bill out of House Rules—Representative Rodney Tom (R during the 2006 legislation year. He switched to D on March 14, 2006)
Place on the House Floor agenda—Representative Frank Chopp (D)
Sign the bill into law—governor.
Step 8
The Washington State Urological Society executive director coordinated society members to participate.
Men’s Health Committee member provided scientific references to state senator introducing legislation.
Men’s Health Committee member provided testimony at the Senate Health and Long-Term Care Committee hearing Jan. 9, 2006.
Membership was broken down into legislative districts. Strategic committee members and people influencing the flow of the legislative process were identified.
Washington State Urological Society members communicated at strategic times in the legislative process to their state senators and house representative. (eg, President Jeff Frankel, MD, phoned the chairwoman of the House Healthcare Committee as a constituent requesting her to put the bill up for Executive Session). Phone calls were made, and e-mails and faxes were sent.
Step 9
Constant follow-up was made by the executive director of the Washington State Urology Society. Every action was provided a thank you and follow-up. Legislators were asked advice on how to move the bill further in the process. Every thank you and follow-up included visual reminders of the legislation (eg, the family pin, National Prostate Cancer Coalition (NPCC) wrist bands, PCa awareness pins).
A timeline summary is as follows
November 2005—strategy created and funding requests were drafted
July 23, 2006—Safe-At-Home: A Health Project of Us Too International took place at the Senior Softball USA Western Regional Tournament
August 2006—film editing completed and follow-up with senators
September to November 2006—follow-up with senators on commitment of introducing men’s health legislation this session
December 2006—provide draft legislation to senator at his request (NPCC provided); Washington State Urological Society Men’s Health Committee member provided PSA supporting documentation; society’s executive director provided state-specific statistics concerning PCa
January 2007
3—bill was filed and provided number
9—Senate Healthcare Committee hearing (AACU provided testimony)
26—Voted out of Senate Healthcare Committee
30—substitute bill passed to Senate Rules Committee
February 2007
2—pulled out of Rules
8—Voted out of the senate 42 yeas, 1 nay, 2 absent, 4 excused
10—House Healthcare Committee hearing first reading
17—House Healthcare Committee hearing (included AACU testimony)
21—voted out of Healthcare Committee and referred to Appropriations
23—Appropriations Hearing (included AACU testimony)
24—passed to Rules without appropriation because the $50,000 was not in the House budget although it was in the Senate Budget
28—pulled out of Rules Committee
March 2007
1—voted out of the House with 86 yeas, 12 nays
4—Senate concurred with House amendment to remove appropriation
7—president signed and speaker signed
8—delivered to the governor
30—tentative date for governor signature
Benefits of the legislation include
Increased informed decision making between physicians and their patients
Physicians able to screen patients for prostate cancer regardless of age if they feel it is medically necessary and have it covered by health insurance
$50,000 placed into the state budget for PCa awareness education; although small, it is viewed as a start in the dialog for future funding needs in this area.
Washington State Urology Society pearls for other state societies include
Work closely with the AACU on state issues.
Get actively involved in the State Society Network to enhance success rates.
Include strategic legislative representatives to participate at state meetings.
Invite legislators (state and federal) to come to one’s practice during the nonsession months.
Keep an ongoing dialog with representatives and senators.
Get networked with the government affairs managers of urology venders such as TAP Pharmaceuticals (now known as Abbott Laboratories; North Chicago, IL, USA) and Novartis (East Hanover, NJ, USA).
Include patient advocacy groups in legislative efforts both within the state and on a federal basis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






