The prescription of chronic peritoneal dialysis involves a number of elements. Initially, there is the choice of peritoneal dialysis modality between continuous ambulatory peritoneal dialysis (CAPD) and cycler or automated peritoneal dialysis (APD) and their variants. Then there is the selection of a specific prescription based on clearance, ultrafiltration, and nutritional/metabolic requirements. The term “adequacy” is often used in this context and usually refers specifically to the quantity of clearance delivered but can also be used in a broader sense to reflect the quality of the dialysis prescription as a whole. Please review Chapter 21 (Physiology) and 22 (Equipment) at this time, as many concepts discussed in those chapters will not be repeated here.
I. CHOICE OF A PERITONEAL DIALYSIS (PD) TREATMENT MODALITY (Table 25.1, Fig. 25.1)
A. Modalities of peritoneal dialysis therapy
1. CAPD. The simplicity of CAPD, the ease of doing it at home, its relatively low cost, and the associated freedom from dialysis machinery have combined to make it historically the most popular chronic peritoneal dialysis modality. It provides continuous therapy and a steady physiologic state. Control of body fluid volume can usually be achieved, and normalization of blood pressure is possible in most patients.
The principal disadvantage of CAPD for many patients is the requirement for multiple procedural sessions (usually four per day), each taking up 30–40 minutes of patient time. While these can be done away from home, the requirement for sterility and access to supplies usually means that the patient returns home, and so this may constrain daily activities somewhat. Frequency of procedures may also be an issue where relatives or other caregivers are carrying out the exchanges for the patient. Other factors are limitations on dwell volumes due to increased intraperitoneal pressure and a limited range of solute clearance. Episodes of peritonitis occurring as often as once every 12 months were a significant disadvantage in the past; however, with improved transfer sets and connecting devices, such occurrences have been markedly reduced and successful programs report rates of one peritonitis episode every 3 years or fewer.
Comparison of Typical CAPD and APD Prescriptions | |
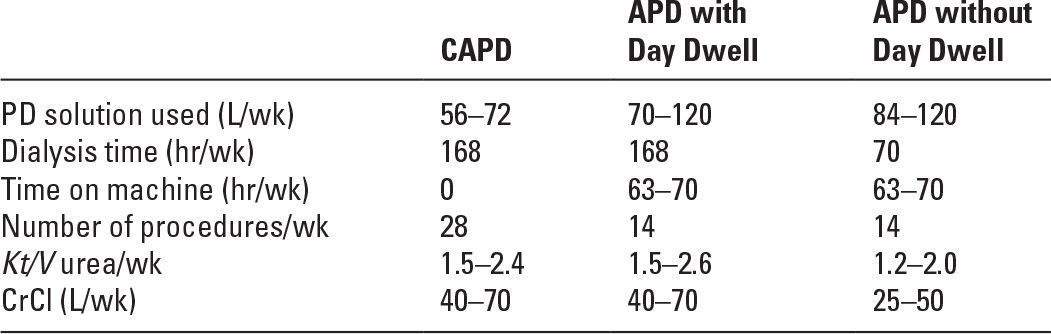
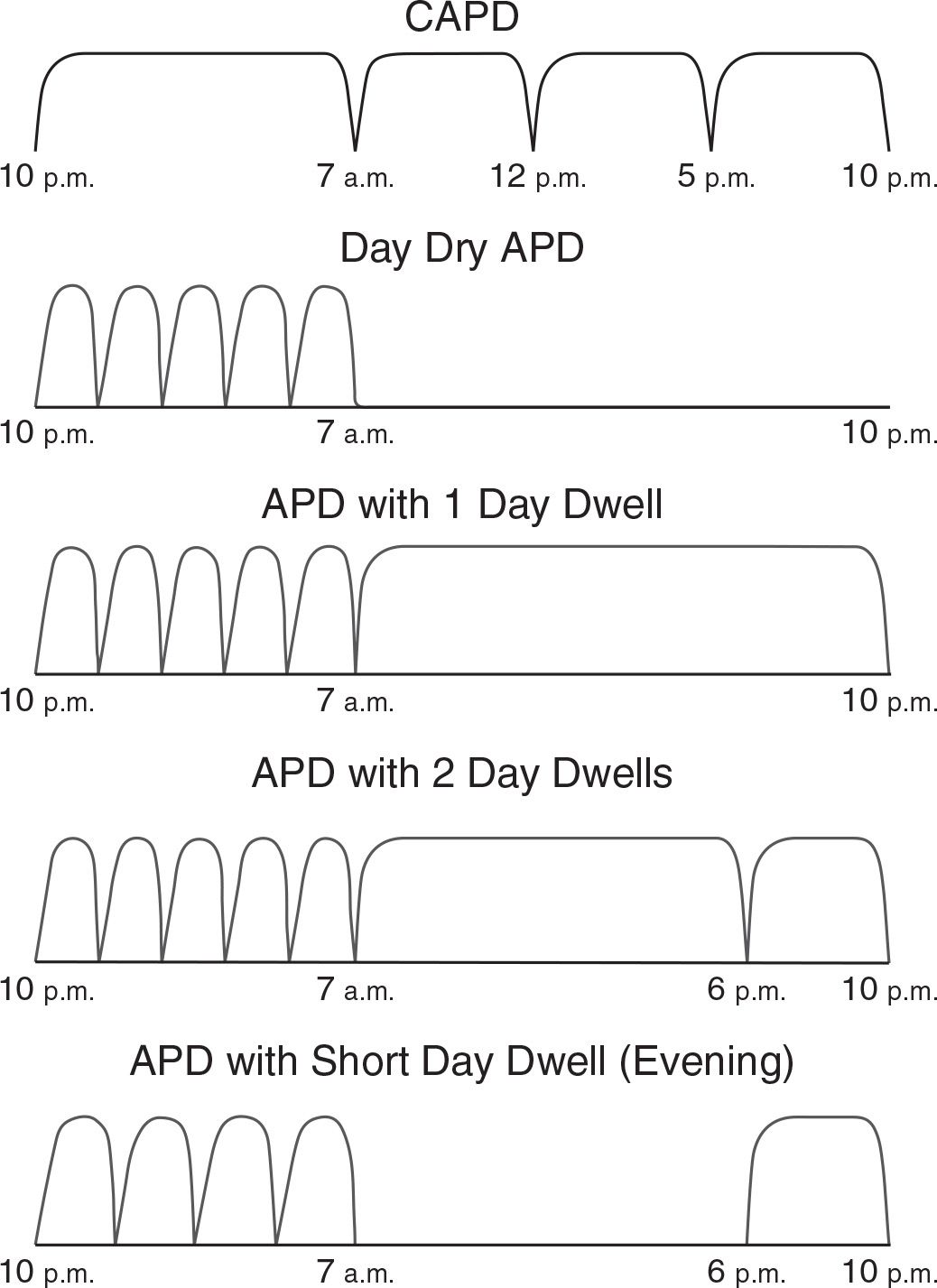
FIGURE 25.1 Diagrammatic representation of various CAPD and APD prescriptions.
2. APD.This has become very popular over the past 10–15 years and, in many wealthier countries, is being used in the majority of peritoneal dialysis patients. The main advantage of APD, compared with CAPD, is the lesser number of on–off procedures required each day—typically two versus four for CAPD—and none during the daytime. All connections and preparation of equipment usually take place in the privacy of the home so that psychological adjustment is facilitated and patient fatigue and “burnout” may be reduced. APD is an attractive treatment option for active individuals who would be inconvenienced by the interruptions in daily routine that are required with CAPD. APD is also the therapy of choice for most patients who require assistance in carrying out their dialysis (e.g., children, the dependent elderly, and nursing home residents).
The main disadvantages of APD relative to CAPD are the need for a cycler, the greater cost, and the slightly greater complexity.
APD has classically been divided into APD with a day dwell, often called continuous cycling peritoneal dialysis (CCPD), and day dry APD (Fig. 25.1), often called nocturnal intermittent peritoneal dialysis (NIPD). These modalities have already been described in Chapters 21 and 22.
An alternative form of APD is tidal peritoneal dialysis (TPD). This modality uses an initial fill volume followed by partial drainage at periodic intervals (Fernando, 2006). The principal purpose of TPD was to enhance clearance of small solutes by avoiding the normal loss of dialysis time associated with inflow and drainage. In terms of clearance, the advantage of TPD over standard APD is not seen unless very large quantities of dialysis solution are used. The main use of TPD nowadays is to minimize drain pain during nighttime cycling. The main disadvantage of high-volume TPD is increased cost and complexity, and it is not widely used.
B. CAPD or APD: Which modality to choose? This decision should take into consideration both patient preferences and the need to provide a medically optimal peritoneal dialysis prescription. Patient preferences may be based on lifestyle, employment, place of residence, ability to perform the various modalities of PD, comfort with cycler technology, and the degree of family and social support. In the past, peritoneal transport status and its influence on clearance and fluid removal were thought to be critical in choosing between CAPD and the different types of APD, but there is now an increasing sense that these aspects were overstated and that lifestyle factors should be given more emphasis.
APD was previously thought to be better than CAPD for managing volume status. However, the phenomenon of sodium sieving (see Chapter 26) is more apparent with the short-cycled dwell times of APD, and this, along with the risk of net fluid resorption with long day dwells, has led to concerns about adequacy of sodium removal with APD. One recent study suggests less salt removal and a higher prevalence of systolic hypertension with APD than with CAPD, but this was not a randomized trial, and there is no consensus that these findings are generalizable (Rodriguez-Carmona, 2004). Salt and water removal require close attention on both CAPD and APD, but there is insufficient evidence to justify it being a factor in initial modality selection.
Risk of peritonitis is another medical factor that may arise when deciding between CAPD and the variants of APD. One randomized trial done over two decades ago showed less peritonitis on APD, but both modalities have changed since then, and there is now no consensus that one or the other is more likely to predispose to peritonitis.
A third consideration is cost. CAPD generally is cheaper than APD. Dialysis programs have to deal with financial constraints, and in some settings, patients may have to bear some or all of the costs.
II. CHOICE OF A PRESCRIPTION
A. Clearance targets
1. Weekly Kt/V urea. Clearance targets in PD are set in terms of weekly urea clearance (Kt) normalized to the patient’s estimated urea distribution volume (V). Current guidelines aim for a Kt/V urea target of at least 1.7. Previously, this target had been set higher, at 2.0 or even greater for noncontinuous forms of PD, but the guidelines were lowered based on further trial evidence, and in particular, the randomized ADEMEX study (Paniagua, 2002), which found no difference in outcomes between patients assigned to receive a higher versus a lower dose of PD. In the ADEMEX trial, the average weekly Kt/V was 2.1 in the patients assigned to more dialysis, compared to 1.6 in the lower-dose group. Current guidelines do not set different targets for continuous and noncontinuous forms of PD (e.g., day dry APD), nor do they set different targets based on peritoneal transport status. A similar trial from Hong Kong (Lo, 2003) also failed to find a benefit of higher doses of PD.
2. Weekly creatinine clearance (CrCl) per 1.73 m2. Previous guidelines also set a weekly CrCl target in addition to the Kt/V urea target. The creatinine target was normalized to 1.73 m2 body surface area and was in the range of 60/1.73 m2 L per week. The idea of setting a separate creatinine target was to model a uremic toxin that had slightly higher molecular weight than urea (113 vs. 60 Da) and that was not so rapidly removed by diffusion. Most current guidelines no longer recommend a minimum level of weekly CrCl as such targets have not been shown to be of any additional value over Kt/V targets. However, they do reflect clearance of slightly larger molecules than urea, and so European, but not US, guidelines suggest an additional CrCl target of 45/1.73 m2 L per week (Dombros, 2005).
3. Should residual kidney function be counted in the adequacy target? Greater residual renal clearance has repeatedly been shown to be associated with superior patient survival; in fact, it has been difficult to show a similar survival effect for peritoneal clearance, at least within the range of prescriptions in typical clinical use (Churchill, 1995). Some have suggested that the weekly Kt/V urea target of 1.7 should be met by peritoneal clearance alone and that residual renal clearance should be treated as a precious bonus. KDOQI, Canadian, and European guidelines, however, all recommend that peritoneal and renal Kt/V can be added to achieve the target.
4. Same Kt/V target for CAPD and APD. The previous idea that target clearances for APD should be higher than those for CAPD because APD is somewhat more intermittent is now thought to be unjustified and to introduce unnecessary complexity.
B. Measurement of clearance (Table 25.2). Clearance in peritoneal dialysis can be measured in terms of Kt/V urea and additionally as CrCl/1.73 m2. Both clearances comprise a peritoneal and a residual kidney component. Residual kidney function lasts longer in PD than in hemodialysis and accounts for a greater proportion of total clearance.
Formulas for Calculating Clearance Indices in Peritoneal Dialysis | |
Kt/V:
Kt = Total Kt = peritoneal Kt + renal Kt
Peritoneal Kt = 24-hr dialysate urea nitrogen content/serum urea nitrogen
Renal Kt = 24-hr urine urea nitrogen content/serum urea nitrogen
V (by Watson formula):
V = 2.447 – 0.09516 A + 0.1704 H + 0.3362 W (in males)
V = –2.097 + 0.1069 H + 0.2466 W (in females)
where A = age (y); H = height (cm), and W = weight (kg)a
CrCl:
CrCl = total CrCl corrected for 1.73 m2 BSA
Total CrCl = peritoneal CrCl + renal CrCl
Peritoneal CrCl = 24-hr dialysate creatinine content/serum creatinine
Renal CrClb = 0.5 (24-hr urine creatinine content/serum creatinine + 24-hr urine urea nitrogen content/serum urea nitrogen)
BSA (DuBois formula):
BSA (m2) = 0.007184 × W0.425 × H0.725
where BSA = body surface area (m2), W = weight (kg)a and H = height (cm)
aAnthropometric (median standard or ideal body weight as per Appendix B) instead of actual body weight may be used for calculation of V or BSA.
bFor PD adequacy purposes, renal “CrCl” is the average of the urinary creatinine and urea creatinine clearances.
1. Measurement of weekly Kt/V urea. Peritoneal Kt/V is calculated by performance of a 24-hour collection of dialysate effluent and measurement of its urea content. This is then divided by the average plasma urea level for the same 24-hour period to give a clearance term, Kt (Table 25.3). The timing of the plasma urea sample is not critical in CAPD because it is relatively constant at all times. In APD, blood urea is not quite so constant throughout the day; ideally, therefore, it is best to take a measurement in the middle of the noncycling daytime period, which is typically between 1:00 p.m. and 5:00 p.m. and is thought to represent approximately the average blood urea levels for the day.
Residual renal Kt urea is calculated in the same way using a 24-hour collection of urine. The two (peritoneal and renal) Kt terms are then combined to give total Kt per day, and this value is normalized to V, which represents total body water. It is recommended that V be estimated using one of the standard formulas for total body water, such as those of Watson or of Hume–Weyers. These are based on patient age, sex, height, and weight (Table 25.2). This then gives a daily value for Kt/V urea, which then needs to be multiplied by 7 to give a weekly value. In the calculation of V, normalization of Kt to the patient’s ideal or standard V (calculated using the ideal or standard body weight as described in Appendix B) rather than actual V (calculated from actual body weight) is recommended. This makes it easier to achieve targets in obese patients and is appropriate, in that most do not believe that clearance requirements should rise in proportion to body fat. Conversely, wasted malnourished patients will require more dialysis to achieve targets if clearance is corrected to their standard or ideal body weight. These weights are calculated from anthropometric values, as described in Appendix B, and then the standard or ideal body weight value should be used in the Watson equation to calculate the value for an adjusted V.
Examples of Clearance Calculations in CAPD and APD | |
1. A 50-year-old man weighing 66 kg has no residual renal function. He is on CAPD with four 2.5-L exchanges daily, and his net UF is 1.5 L. His V by the Watson formula is 36 L, and his BSA by the DuBois formula is 1.66 m2. Serum urea nitrogen is 70 mg/dL (25 mmol/L), and serum creatinine is 10 mg/dL (884 mcmol/L). The urea nitrogen and creatinine (after correction for glucose) levels in the 24-hr dialysate collection are 63 mg/dL (22.5 mmol/L) and 6.5 mg/dL (575 mcmol/L), respectively. Calculate his Kt/V and CrCl.
Kt urea/d = 24-hr drain volume × D/P urea = 11.5 L × 63/70 = 10.35 L/d. Daily Kt/V = 10.35 L/36 L = 0.288
Weekly Kt/V = 0.288 × 7 = 2.02
Creatinine clearance per day = 24-hr drain volume × D/P creatinine = 11.5 L × 6.5/10 = 7.48 L/d. Corrected for 1.73 m2 BSA = 7.48 × 1.73/1.66 = 7.80 L/d. Weekly CrCl/1.73 m2 = 7.8 × 7 = 55 L/wk.
2. A 48-year-old woman on APD weighs 63 kg and does five 2.4-L cycles nightly plus a 6-hr 2-L day dwell. Her V by Watson is 32 L, and her BSA by DuBois is 1.60 m2. Her 24-hr dialysate drain volume is 15 L, indicating 1 L net UF. Her pooled dialysate collection has a urea nitrogen level of 48 mg/dL (17.1 mmol/L) and a creatinine level (after correction for glucose) of 4.5 mg/dL (398 mcmol/L). Her mid-afternoon serum urea nitrogen is 65 mg/dL (23.2 mmol/L), and serum creatinine is 9 mg/dL (796 mcmol/L). Her urinary urea and creatinine clearance are 2 and 4 mL/min, respectively.
Calculate her total weekly Kt/V and creatinine clearance.
Peritoneal Kt = daily drain volume × D/P urea = 15 L × 48/65 = 11.1 L. Peritoneal Kt/V = 11.1 L/32 L = 0.35/d = 2.45/wk.
Renal urea clearance = renal Kt urea = 2 mL/min = 20 L/wk. Renal Kt/V = 20/32 = 0.63/wk.
Total Kt/V = peritoneal plus renal Kt/V = 2.45 + 0.63 = 3.08/wk
Peritoneal creatinine clearance = daily drain volume × D/P creatinine = 15 L × 4.5/9 = 7.5 L. Corrected for 1.73 m2 BSA = 7.5 × 1.73/1.60 = 8.1 L/d = 57 L/wk.
Renal creatinine clearance (for this purpose) = mean of renal urea and renal creatinine clearance = mean of 2 and 4 mL/min = 3 mL/min = 30 L/wk. Corrected for 1.73 m2 BSA = 30 × 1.73/1.60 = 32.4 L/wk.
Total creatinine clearance/1.73 m2 = 57 + 32.4 = 89.4 L/wk.
D/P, dialysate/plasma; UF, ultrafiltration.
2. Measurement of weekly CrCl/1.73 m2. The measurement of CrCl is similar to that of Kt/V (Tables 25.2 and 25.3). Again, the peritoneal component is calculated by measuring the creatinine content of a 24-hour collection of dialysate effluent, and this is then divided by the serum creatinine. The way that renal CrCl is added to the peritoneal component differs from the procedure for Kt/V urea. Residual renal CrCl is known to markedly overestimate true glomerular filtration rate in most patients; therefore, it is conventional to add the average of the urinary urea and creatinine clearances to the peritoneal clearance to give the total CrCl. The total daily “creatinine clearance” is then normalized to 1.73 m2 body surface area (BSA), with BSA estimated using the formula of DuBois or Gehan and George (see Appendix B). This daily clearance value is then multiplied by 7 to give a weekly CrCl/1.73 m2. Normalization to standard or ideal body weight can be done in the same way as for Kt/V urea, where the weight from Appendix B is used to calculate an adjusted BSA value.
a. Analytical problem in measuring creatinine in glucose-containing dialysate. The high glucose levels found in dialysate artifactually elevate the measurement of creatinine in some biochemical assays, and each laboratory should make a correction for this based on its own experience. This may be done by spiking unused bags of dialysis solution containing various dextrose concentrations with a known amount of creatinine and then performing the assay, enabling derivation of the appropriate correction factor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





