Abdominal and Pelvic Protocol Basics
All of the preceding information in this text serves primarily to provide the reader with the necessary tools to establish and understand magnetic resonance (MR) protocols for the abdomen and pelvis and to modify those protocols to ensure that diagnostically useful images are obtained within a reasonable amount of time. Due to hardware and software variations among different MR systems, no single textbook can provide detailed MR imaging (MRI) protocols that can be directly applied to every scanner. Individuals have their own tolerance or preferences for image noise, artifacts, scan time, and imaging planes. Any attempt to provide detailed vendor-specific protocols would please a few individuals while frustrating most others. Therefore, the following discussion provides generic versions of abdominal and pelvic protocols that can be used to develop specific protocols for unique practice situations. First, the most commonly used sequences for abdominal and pelvic imaging are reviewed, then a framework for specific clinical scenarios is provided to serve as a starting point for protocol development. We purposely omit parameters that must be individualized for each patient, such as field of view (FOV). Also note that specific parameters such as the repetition time (TR) and echo time (TE) vary according to personal preference, scanner type, desired imaging time, and field strength. The numbers provided herein should only serve as a starting point. We assume a field strength of 1.5 tesla (T) throughout, because this value is commonly used for abdominal and pelvic work. However, most of the principles presented herein are equally relevant to scanning at lower or higher clinically available field strengths.
We believe that many abdominal and pelvic MRI examinations require some degree of monitoring by a knowledgeable individual to ensure a diagnostically useful study is done. This monitoring allows additional sequences or imaging planes to be performed to best demonstrate pertinent anatomy or characterize lesions. In addition, because patient compliance varies considerably, protocol modifications may be necessary to accommodate a patient’s clinical status.
Commonly used Sequences
Most MR protocols for the abdomen and pelvis contain a combination of T1- and T2-weighted sequences. The following discussion reviews the advantages and disadvantages of various T1- and T2-weighted techniques.
T1-Weighted Sequences
Spin Echo
Uses: T1-weighted non-breath-hold imaging of the abdomen and pelvis.
Strengths: High-resolution T1-weighted imaging is possible when motion is not a problem.
Weaknesses: Motion artifacts are difficult to completely eliminate. Sequences are time consuming.
Parameters: Most T1-weighted spin echo sequences use a TR of less than 500 msec and a TE as low as possible. Up to four signal averages are typically used. A rectangular FOV with anterior-posterior phase-encoding direction is most time efficient.
Echo Train Spin Echo (FSE, TSE)
Uses: T1-weighted imaging of the pelvis.
Strengths: A good compromise between spin echo and gradient echo in terms of image quality and scan time.
Weaknesses: Relatively few slices can be obtained during a single breath-hold.
Parameters: TR and TE should be kept as low as possible. A typical sequence has a TR of less than 500 msec and TE of 12 to 15 msec. The echo train length is commonly set at 3 but can be adjusted (with adjustments in the TR).
Two-Dimensional Spoiled Gradient Echo (FLASH, T1FFE, SPGR)
Uses: Breath-hold T1-weighted imaging of the abdomen and pelvis, often with in-phase and opposed-phase echo times.
Strengths: Breath-hold in-phase and opposed-phase imaging possible.
Weaknesses: Lower signal-to-noise ratio than spin echo techniques. Susceptibility artifact is more apparent.
Parameters: For in-phase imaging, the TR is usually 100 to 150 msec with the TE set at 4 to 4.5 msec. For opposed-phase imaging, the TE is set at 1.9 to 2.3 msec. Dual-echo sequences allow in-phase and opposed-phase echoes to be acquired during one TR and are usually preset for the appropriate echo times. The TR may be adjusted to accommodate modifications in other scan parameters. A flip angle of 70 to 80 degrees allows for adequate T1-weighted contrast and signal. Because these are breath-hold sequences, multiple signal averages are not used. The sampling bandwidth can be adjusted to alter scan time, image noise, or chemical shift artifact.
Three-Dimensional Spoiled Gradient Echo (VIBE)
Uses: Breath-hold dynamic contrast-enhanced imaging of the abdomen and pelvis.
Strengths: Allows rapid imaging with high through-plane spatial resolution. Isotropic voxel size can be achieved on some scanners, allowing high-quality vascular reconstructions in any plane.
Weaknesses: Motion causes degradation of entire data set.
Parameters: TR and TE should be minimized (TR< 5 msec, TE< 2 msec). A low flip angle (e.g., 15 degrees) allows for adequate T1 contrast. Zerofill interpolation is routinely used.
T2-Weighted Techniques
Half-Fourier Single-Shot Echo Train Spin Echo (HASTE, ssTSE, ssFSE)
Uses: Breath-hold localizer, rapid abdominal survey, fetal imaging, MR cholangiopancreatography (MRCP), bowel imaging, and MR urography.
Strengths: Very resistant to motion and susceptibility artifact. Cysts and hemangiomas appear very bright. Imaging times are brief (approximately 1 second or less per image).
Weaknesses: Images limited by relatively low signal-to-noise ratio and blurring. Malignant lesions within solid organs may be less conspicuous.
Parameters: The TR is infinite, because the excitation pulse is applied only once per image. The TE can be adjusted as desired. A short TE (40 to 60 msec) provides the best signal-to-noise ratio. A longer TE may be desirable in some cases for imaging fluid-filled structures. Flow artifacts may be accentuated with a longer TE. Generally, a single signal average and a flip angle of 150 to 180 degrees are used.
Echo Train Spin Echo (FSE, TSE)
Uses: Non-breath-hold imaging of the abdomen and pelvis.
Strengths: Good signal-to-noise ratio, good contrast-to-noise ratio.
Weaknesses: Time consuming. Image quality limited by motion unless some type of respiratory compensation (e.g., triggering) is used.
Parameters: For most abdominal and pelvic applications, the TR should be 2,000 to 5,000 msec and the TE should be 70 to 90 msec. The TR can be adjusted within this range to accommodate other parameter modifications. An echo train length of 8 to 16 with up to four signal averages is commonly used.
GraSE
Uses: General T2-weighted imaging of the abdomen.
Strengths: Relatively quick. Lower specific absorption rate than echo train spin echo techniques.
Weaknesses: Not widely available, limited clinical experience.
Parameters: A TR of 1,800 works well for most applications. Adjust the TE as for a fast spin echo sequence. Two signal averages, an echo train length of 14, and an EPI factor of 3 (i.e., the number of gradient echoes per spin echo) provide images similar to a standard echo train spin echo sequence.
TurboSTIR
Uses: Breath-hold fat-suppressed T2-weighted imaging of the abdomen.
Strengths: Covers most organs in one or two breath-holds. Uniform fat suppression can be achieved. Good lesion conspicuity in solid organs.
Weaknesses: Relatively low signal-to-noise ratio.
Parameters: A TR of 3,800 msec, TE of 70 to 80 msec, flip angle of 150 degrees, and an inversion time (TI) (for fat suppression) of 165 msec works well for most applications.
Abdominal and Pelvic Protocols
The following are examples of abdominal and pelvic protocols to serve as a starting point. We recommend using a phased-array surface coil whenever possible, although it is difficult to cover the entire abdomen and pelvis in a single FOV with most commercially available surface coils. For this reason, it is usually not possible to perform high-quality, contrast-enhanced dynamic MRI of both the abdomen and pelvis in the axial plane with a phased-array surface coil. If contrast-enhanced imaging of both the abdomen and pelvis is desired during a single session, one must determine where dynamic imaging will be most useful. In addition, each time a different anatomic region is examined, the surface coil must be repositioned and new localizer images obtained. In the rare case when high-quality dynamic imaging of both the
abdomen and pelvis is required, it may be necessary to schedule the patient for examinations on two different days, because persistent enhancement of some anatomic structures from the first dynamic study may impact the quality of a second contrast-enhanced examination performed without sufficient delay.
abdomen and pelvis is required, it may be necessary to schedule the patient for examinations on two different days, because persistent enhancement of some anatomic structures from the first dynamic study may impact the quality of a second contrast-enhanced examination performed without sufficient delay.
Basic Abdominal Protocol
General comments: Many abdominal protocols are slight variations of a simple protocol (Fig. 1.43) such as that below. We have found this protocol to be effective for the majority of liver, pancreas, adrenal, and renal examinations. When developing a protocol, it may be helpful to start with this one, modifying it to suit the specific clinical scenario. Additional information on specific techniques such as MR angiography (MRA), MRCP, and MR urography is provided in Section 2.
Breath-hold localizer: HASTE/ssFSE/ssTSE
Purpose: General survey, breath-hold localizer
Respiratory: Breath-hold
Imaging plane: Coronal
Slice thickness: 8 mm
In-phase and opposed-phase T1: Dual-echo spoiled gradient echo
Purpose: Characterization of lipid-containing lesions
Respiratory: Breath-hold
Imaging plane: Axial
Slice thickness: 6 to 8 mm
Fat-suppressed T2: FSE/TSE, GraSE, or turboSTIR
Purpose: Lesion characterization, detection of lymphadenopathy and fluid
Respiratory: Breath-hold for turboSTIR; triggered for FSE or GraSE
Imaging plane: Axial
Slice thickness: 6 to 8 mm
Dynamic gadolinium-enhanced T1: 2D or 3D spoiled gradient echo (fat-suppressed if possible)
Purpose: Lesion detection and characterization; depiction of vascular anatomy
Respiratory: Breath-hold (expiration preferred)
Imaging plane: Axial
Slice thickness: 6 to 8 mm (2D),<5 mm (3D)
Injection rate and volume: 2 mL/sec for 20 mL
Initial scan delay: Based on test bolus and organ of interest
Number of scans: Precontrast, arterial, venous (45 seconds), equilibrium (90 seconds)
Delayed fat-suppressed T1: 2D or 3D spoiled gradient echo
Purpose: Lesion characterization (particularly hemangioma and cholangiocarcinoma)
Respiratory: Breath-hold (expiration preferred)
Imaging plane: Variable
Slice thickness: Same as dynamic study
Liver Protocol Modifications
Adjust slice thickness, rectangular FOV, and matrix to cover the entire liver in a single breath-hold for breath-hold sequences. In-phase and opposed-phase imaging and breath-hold T2-weighted imaging may be performed in one or two breath-holds to improve image quality.
Optional elements:
Coronal or sagittal imaging for lesions near the liver dome.
MRCP protocol for assessment of bile ducts.
Long TE (≥140 msec) T2-weighted images for characterization of cyst or hemangioma (Fig. 1.44).
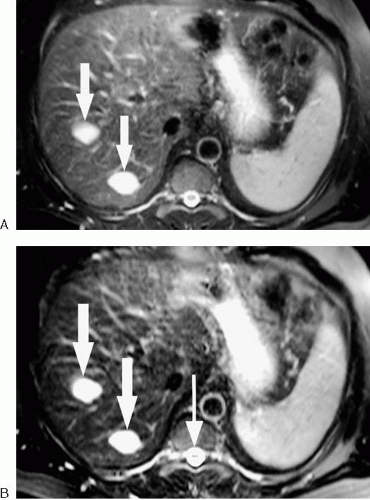 FIG. 1.44. Use of increasing echo time to characterize hepatic lesions. A: Fat-suppressed T2-weighted image (echo time [TE] 80 msec) shows two high signal intensity lesions (arrows) in right hepatic lobe. B: On long TE (160 msec) image, relative signal intensity of liver decreases, but lesions (arrows) remain nearly isointense to cerebrospinal fluid (thin arrow). Therefore, lesions have very long T2 relaxation times compatible with cysts or hemangiomas (in this case, hemangiomas).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|