disease commonly produces blood loss. Anorectal neuromuscular function is tested by assessing basal anal tone, adequacy of maximal anal squeeze, and perianal cutaneous sensation, including the anal wink. Long-standing constipation with straining and prolapse may produce anal or perineal nerve damage that leads to reduced anal pressure and fecal incontinence. Examination during attempted defecation maneuvers can suggest rectal prolapse and evidence of rectosphincteric dyssynergia. Pelvic examination in women may demonstrate a rectocele with straining.
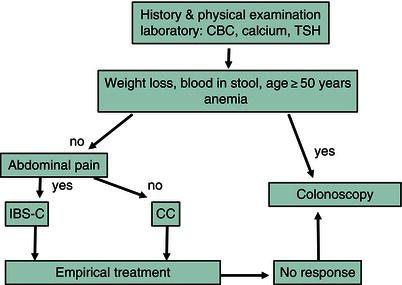
Figure 9.1 Constipation. CBC, complete blood count; CC, chronic constipation; IBS-C, irritable bowel syndrome-constipation predominant; TSH, thyroid-stimulating hormone.
Additional testing
Laboratory studies
If the history or examination suggests systemic or local anorectal disease, further evaluation may be needed (Figure 9.1). A microcytic anemia raises concern for colonic neoplasm or inflammatory disease. Other screening tests include measuring serum calcium to exclude hyperparathyroidism and thyroid-stimulating hormone levels to exclude hypothyroidism. Specific serological tests can detect rheumatological disease, Chagas disease, or paraneoplastic pseudo-obstruction, whereas other assays are used for catecholamines, porphyrins, and glucagon.
Structural studies
Endoscopic or radiographic evaluation is performed on any individual with suspected mechanical obstruction as a cause of constipation. In young patients, flexible sigmoidoscopy is sufficient. For patients older than 40–45 years or if alarm findings such as bleeding are present, it is important to evaluate the entire colon by colonoscopy because of the increased risk of colorectal neoplasm. Computed tomography (CT) scans or barium enema radiography can show proximal colonic dilation as well as persistent contraction of the denervated segment in Hirschsprung disease. Deep rectal biopsy specimens obtained at least 3 cm above the anal verge are obtained to exclude Hirschsprung disease, when indicated.
Functional studies
In young patients without alarm symptoms, or patients in whom structural diseases have been excluded, empirical trials of medical therapy are offered. For a patient whose condition is refractory to standard treatment, additional evaluation may be indicated to assess the functional integrity of the colon and anorectum. Anorectal manometry with balloon expulsion should be performed in patients with chronic constipation who do not respond to empirical medical therapy. The transit of stool through different colonic regions can be quantified by obtaining serial abdominal radiographs after ingesting radio-opaque markers, or by newer technology involving a swallowed capsule that measures pH, temperature, and intralumenal pressure to determine intestinal transit time. These studies can distinguish between slow-transit constipation (colonic inertia), in which transit is delayed in all colonic regions, and functional outlet obstruction, where passage is selectively retarded at the level of the anorectum. In some cases, marker elimination is normal, even though the patient denies stool output. Such individuals often exhibit psychological disturbances that contribute to their symptoms.
Differential diagnosis
The causes of constipation are numerous, including secondary causes and idiopathic disorders, and relate to either impairment of colonic transit or to structural or functional obstruction to fecal evacuation (Table 9.1).
Mechanical colonic obstruction
Colonic obstruction may result from mechanical narrowing of the distal colon or anus or from functional outlet obstruction. The most important mechanical cause is colon carcinoma, which typically presents in individuals over age 50 or in selected high-risk groups. Although colon cancer often presents with gross or occult fecal bleeding, a subtle decrease in stool frequency or caliber for weeks to months may be the only initial complaint. Benign colonic strictures resulting from diverticulitis, ischemia, or inflammatory bowel disease produce similar symptoms. Anal strictures, foreign bodies, or spasm from painful fissures or hemorrhoids also may interrupt stool expulsion.
Neuropathic and myopathic disorders
Diseases of the extrinsic or enteric innervation of the colon and anus may produce constipation. Constipation may be caused by transection of the sacral nerves or cauda equina, lumbosacral spinal injury, meningomyelocele, or low spinal anesthesia. These may lead to colonic hypomotility and dilation, decreased rectal tone and sensation, and impaired defecation. Colonic reflexes are preserved with high spinal lesions; thus, digital stimulation can trigger defecation. However, patients with spinal injury have reduced meal-induced colonic motor activity and impaired rectal sensation and compliance that can contribute to constipation. Constipation is prevalent with multiple sclerosis, cerebrovascular accidents, Parkinson disease, and dysautonomias, including Shy–Drager syndrome.
Table 9.1 Causes of constipation
| Colonic obstruction Colorectal neoplasms Benign strictures (e.g. diverticulitis, ischemia) Inflammatory bowel disease Endometriosis Anal strictures or neoplasms Rectal foreign bodies Anal fissures and hemorrhoids Neuropathic and myopathic disorders Peripheral and autonomic neuropathy Hirschsprung disease Chagas disease Neurofibromatosis Ganglioneuromatosis Hypoganglionosis Intestinal pseudo-obstruction Multiple sclerosis Spinal cord lesions Parkinson disease Shy–Drager syndrome Transection of sacral nerves or cauda equina Lumbosacral spinal injury Meningomyelocele Low spinal anesthesia Scleroderma Amyloidosis Polymyositis/dermatomyositis Myotonic dystrophy Metabolic and endocrine disorders Diabetes mellitus Pregnancy Hypercalcemia Hypothyroidism Hypokalemia Porphyria Glucagonoma Panhypopituitarism Pheochromocytoma Medications Opiates Anticholinergics Tricyclic antidepressants Antipsychotics Anti-parkinsonian agents Antihypertensives Ganglionic blockers Vinca alkaloids Anticonvulsants Calcium channel antagonists Iron supplements Aluminum antacids Calcium supplements Barium sulfate Heavy metals (i.e. lead, arsenic, mercury) Idiopathic constipation Colonic inertia Megarectum/megacolon Rectosphincteric dyssynergia Rectocele/rectal prolapse Irritable bowel syndrome |
Hirschsprung disease is the best characterized enteric nervous system disease that presents with constipation. Most commonly, affected infants present with
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






