Overall Bottom Line
- A unique feature of the liver is its dual blood supply via the hepatic artery and portal vein.
- LT requires a minimum of three, and very frequently four, vascular anastomoses to establish inflow and outflow to the allograft.
- Bleeding complications of these anastomoses are readily identified in the operating room, leaving anastomotic stenosis and thrombosis as the leading vascular complications encountered post-operatively.
- Surgical and radiologic approaches play complementary roles in the diagnosis and management of these potentially catastrophic complications and early recognition is key to graft and patient survival.
- Vascular complications following LT generally fall into three categories: hepatic venous, portal venous or arterial complications.
Hepatic Venous Occlusion
Section 1: Background
- Hepatic venous outflow is established via one of two methods depending, in part, on surgeon preference as well as graft type.
- Partial grafts from split livers or living donors, by definition, generally do not include the inferior vena cava and direct anastomosis of the donor hepatic vein(s) to the recipient vena cava is necessary. This ”piggyback” method is generally technically more demanding with smaller anastomoses and likely accounts for the increased incidence of outflow obstruction in these patients.
- Although some centers perform piggyback reconstruction for all allografts, partial and whole, a more common approach is the caval-replacement method in which the donor vena cava is anastomosed directly to the suprahepatic and infrahepatic vena cavae that remain after recipient hepatectomy.
Incidence/prevalence
- The incidence of stenosis of the hepatic vein–caval anastomosis varies from 1 to 6%. This can be due to rotation of the liver graft or true stricture of the anastomosis.
Etiology
- Anastomotic technical error.
- Progressive neointimal hyperplasia.
- Allograft positioning error with torsion or compression of anastomosis.
- A side-to-side cavo-cavoplasty reduces the risk of stenosis.
- Hepatic venous outflow obstruction is more common with the piggyback technique.
Predictive/risk factors
- Partial-liver allografts with piggyback anastomotic technique.
- Budd–Chiari or non-cirrhotic extrahepatic portal vein thrombosis as an indication for OLT.
- Hypercoagulable states.
Section 2: Prevention
Not applicable for this topic.
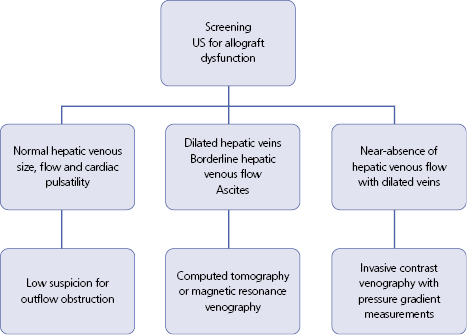
Section 3: Diagnosis (Algorithm 48.1)
Typical presentation
- Hepatic venous thrombosis threatens graft and patient survival due to early parenchymal dysfunction, necrosis and eventual cirrhotic transformation.
- Very early events are usually technical in nature and require re-operation to prevent immediate graft loss.
- With the exception of late, asymptomatic thromboses, all other hepatic venous stenoses and thromboses should undergo invasive imaging by interventional radiology with the intent to perform angioplasty and stenting.
- The technical success rates as measured by minimization of pressure gradients are extremely high, as evidenced by a report of 13 consecutive balloon angioplasties with stent placements. Technical success was achieved in all 13, with clinical success in all but one patient but who subsequently was found to have diffuse, severe hepatic necrosis and underwent re-transplantation.
- Concomitant azotemia and lower extremity edema often indicate at least partial IVC involvement in post-transplantation hepatic venous occlusion. Very frequently these symptoms are due not to inherent IVC stenosis at the anastomotic site, but to compression of the IVC by the distended, enlarged liver. It is for this reason that a period of observation, after balloon angioplasty and stenting of the hepatic venous stenosis to allow time for allograft distention and symptoms of IVC compression to resolve, seems appropriate.
Clinical features
- Hepatomegaly.
- New-onset ascites.
- Abdominal pain.
- Budd–Chiari syndrome.
- Lower extremity edema (with concomitant IVC occlusion or stenosis).
- Renal insufficiency.
Laboratory features
- Elevated transaminases.
- Hypoalbuminemia.
- Prolonged PTT.
- Azotemia (with IVC involvement).
Imaging features
- US always initial diagnostic test to screen for surrogate markers of outflow occlusion:
- Hepatomegaly.
- Ascites.
- Dilated hepatic veins with monophasic flow and loss of cardiac pulsatility.
- Reversal of normal portal hepatofugal flow, becoming hepatopedal in extreme cases.
- Hepatomegaly.
- Contrasted CT and MRI:
- Well-timed studies show excellent detail of hepatic vein/IVC junction.
- Helps to exclude concomitant portal vein stenosis or occlusion.
- Well-timed studies show excellent detail of hepatic vein/IVC junction.
- Invasive venography:
- Imaging offers advantage of direct measurement of pressure gradients across the stenosis from intrahepatic veins to IVC and right atrium.
– – – – – – – – – –
Algorithm 48.1 Screening for allograft dysfunction
– – – – – – – – – –
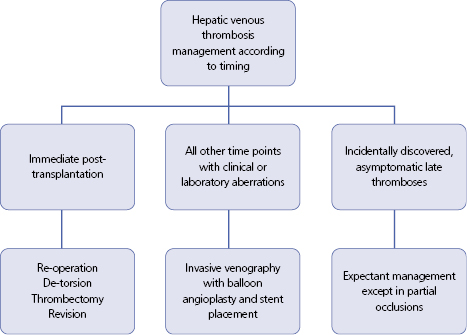
Section 4: Treatment (Algorithm 48.2)
– – – – – – – – – –
Algorithm 48.2 Management of hepatic venous thrombosis