Overall Bottom Line
- Despite landmark advances in surgical techniques and immunosuppression, PNF following LT remains a major cause of early graft and patient loss.
- Though not fully elucidated, the etiology of PNF lies at the intersection of multiple donor and recipient factors and is characterized by immediate coagulopathy, encephalopathy, acidosis, and poor bile production in the absence of a verifiable technical complication such as vascular thrombosis of the graft.
- Though a uniform definition does not exist, graft function insufficient to sustain life leading to death or re-transplantation in the first week post-operatively characterizes the syndrome.
- Despite modifications in organ allocation that allow for emergent re-transplantation in the event of PNF, early patient loss continues to occur because of persistent organ shortage.
Section 1: Background
Definition of disease
- Graft function insufficient to sustain life leading to death or re-transplantation in the first week post-operatively.
- The diagnosis is made within 24–72 hours of transplantation and is based on a combination of clinical and laboratory abnormalities, with confirmation of absence of secondary causes of graft failure such as vascular thrombosis and compression.
Incidence/prevalence
- Clear delineation of the frequency of PNF is difficult to ascertain as definitions vary from center to center, and in cases in which re-transplantation for graft failure occurs, the ultimate outcome of that graft is unknown.
- An incidence of 5% seems to be an accurate approximation, and PNF accounts for roughly one-third of early re-transplantations.
Etiology
- Though not fully elucidated, the etiology of PNF lies at the intersection of multiple donor and recipient factors.
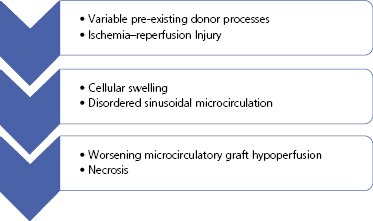
Pathology/pathogenesis (Figure 46.1)
- PNF has been associated with prolonged warm and cold ischemia times as well as donor characteristics such as graft steatosis, donor age and hypernatremia.
- Experimental models of PNF exist specifically for graft steatosis and the effects of reperfusion, but not all cases of PNF involve steatotic grafts.
- The inciting event seems to be ischemia–reperfusion injury alone or in the setting of pre-existing donor processes that leads to cell swelling and disturbance of the hepatic sinusoidal microvasculature.
- Synthetic dysfunction, lactic acid conversion, drug and toxin clearance and bile production are all variably affected.
- Graft necrosis is the ultimate histological outcome in cases of true PNF. Cell swelling and purported disturbance of hepatic sinusoidal microvasculature were demonstrated in an elaborate histopathological study, while ultrastructural changes via electron microscopy have been demonstrated on pre-perfusion biopsies in grafts that ultimately failed.
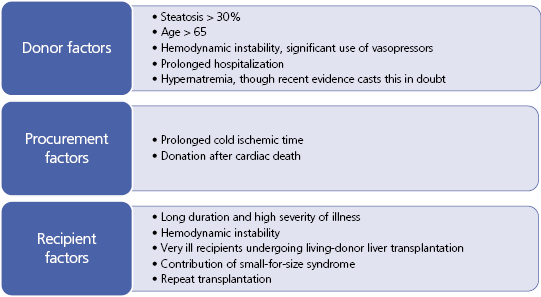
Predictive/risk factors (Figure 46.2)
- Despite multiple identified risk factors, PNF is not completely predictable and involves the interplay of multiple donor, procurement and recipient events.
- Described very early in the age of LT, donor liver steatosis represents one of the most identifiable risk factors for PNF. Frozen-section examination of donor liver biopsies has become standard when suspicion for fatty infiltration exists. Further studies identified macrosteatosis specifically as the dominant risk factor for PNF with the use of fatty livers. Microsteatosis, even severe, is reversible and does not preclude organ usage or predict PNF.
- Unlike kidney transplantation, it is generally well-accepted that the liver does not undergo functional senescence with aging. However, increased donor age seems to be a risk factor for PNF in many observational studies. The severe shortage of donor organs, however, does not preclude the use of older grafts.
- Severe donor hypernatremia, though traditionally associated with worse graft outcomes specifically in terms of PNF following transplantation, has recently been brought into question as a risk factor for PNF. Perhaps more important than absolute hypernatremia is wide fluctuations in sodium concentration in the donors.
- Procurement factors important in minimizing the risk of PNF include shortening the cold ischemic time as much as feasible, especially for marginal organs and when transplanting very ill recipients. The obligatory warm ischemia incurred in donation after cardiac death donors almost certainly contributes to the higher risk of PNF in this donor population.
- Recipient factors are perhaps the least modifiable contributors to PNF. Very ill recipients with high MELD scores, renal failure, and vasopressor requirements represent hostile environments to newly-transplanted grafts. A special scenario unique to living-donor liver transplantation that emulates PNF is small-for-size syndrome in which a partial graft fails to function well in the initial time period following implantation. Native hyperdynamic portal flow to a reduced-size graft leading to portal hyperperfusion is thought to be a major contributor to this phenomenon. Small-for-size syndrome forms the basis for the common practice of denying living-donor liver transplantation to adult patients with advanced disease and severe portal hypertension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree