Overall Bottom Line
- LT is now accepted as a life-saving treatment modality for patients with ESLD or ALF.
- ESLD causes over 75 000 deaths annually in the USA.
- Currently, over 6000 LTs are performed annually in the USA.
- Not all patients, however, are candidates for this procedure; hence the need for an evaluation process.
- A multidisciplinary system is used to evaluate thoroughly the potential LT candidate, including factors that may affect pre- and post-transplantation survival and quality of life.
- The MELD score is currently utilized to prioritize deceased donor organ allocation for LT.
- There continues to be a significant gap between patients who undergo LT and who die while on the waiting list.
Section 1: Background
- The evaluation of patients for LT initially involves identifying patients that would benefit from this procedure.
- Patients undergo a thorough medical, cardiac, surgical and psychosocial assessment.
- The most common disease processes that lead to LT evaluation are listed under “Common etiologies for an LT evaluation.” The majority of patients have ASLD due to cirrhosis from a variety of etiologies. Of those patients that complete the evaluation process and are placed on the waiting list for LT, more than a third have hepatitis C-related liver disease (see table: Patients on the LT waiting list). HCC has become a leading indication as its incidence rises in the USA.
- ALF makes up only 5–10% of all LTs and there are a small number of pediatric and miscellaneous indications.
Common etiologies for an LT evaluation
- Hepatitis C.
- Alcoholic liver disease.
- HCC.
- NASH.
- Hepatitis B.
- ALF.
- Cholestatic liver diseases: PBC, PSC.
- AIH.
- Cryptogenic cirrhosis.
- Metabolic liver diseases: Wilson disease, alpha-1 antitrypsin deficiency, hereditary hemochromatosis.
- Pediatric liver diseases: biliary atresia, primary hyperoxaluria.
Patients on the LT waiting list: UNOS 2010 Annual Report (representing 2009 results). www.unos.org
| Etiology | Percentage |
|---|---|
| Hepatitis C | 30.7 |
| Alcoholic liver disease | 22.6 |
| Malignancy | 4.2 |
| Hepatitis B | 3 |
| ALF | 2.8 |
| Others/cryptogenic | 36.7 |
MELD score
- The MELD scoring system was initially developed at the Mayo Clinic for estimating the 3-month survival of patients with ESLD who underwent TIPS placement.
- A modification of the original MELD score was adapted to predict 90-day survival in patients waiting for LT with a very high accuracy and has subsequently been well validated. The MELD score equation uses the serum bilirubin, creatinine and INR to give a continuous variable. Due to the logarithmic scale used the lowest values for each of the three variables is 1.0 and the creatinine is capped at 4 mg/dL (which is also the value used for patients on renal replacement therapy).
- MELD = 0.378 × loge (bilirubin mg/dL) + 1.12 × loge (INR) + 0.957 × loge (creatinine mg/dL) + 0.643; range: 6–40 points.
- The higher the score, the greater the risk of dying and hence a higher priority for LT. Research has shown that both hospitalized and historical patient groups with a MELD score higher than 40 had a 3-month mortality of 100%.
- The MELD score has been used for deceased donor liver allocation for adult patients in the USA since 2002. A different system (the PELD score) is used for pediatric patients and is detailed in Chapter 38.
- The MELD score accurately predicts waiting list mortality but importantly a higher MELD score does not significantly worsen post-transplantation survival (unless the MELD score is very high). Since some patients would benefit from LT but do not necessarily have ESLD, or have other complications of liver disease that are not considered in the MELD score, a MELD exception can be used. The most common reason for a MELD exception is HCC. A seminal study from Milan by Mazzaferro et al. in 1996 observed that a 4-year survival rate of 65% in LT recipients was noted if certain factors (the Milan criteria) were met.
Milan criteria
- One lesion, between 2 and 5 cm in diameter.
- Up to three lesions, each ≤3 cm in diameter.
- No vascular invasion.
- No metastatic disease.
- Patients with HCC within the Milan criteria are eligible for a MELD exception of 22 points, regardless of their actual MELD score. This MELD exception score is increased by 10% every 3 months and hence it is important to identify HCC in LT candidates as this increases their chance of receiving a LT.
- Several other HCC criteria exist which have tried to increase the number of patients eligible for a MELD exception. The UCSF criteria expands the limits set by the Milan criteria. Although some reports demonstrate similar post-transplantation survival, these criteria are currently not established as the standard by UNOS:
- UCSF criteria:
- One lesion, up to 6.5 cm in diameter.
- Up to three lesions, each not exceeding 4.5 cm in diameter.
- Total tumor diameter not exceeding 8 cm.
- No evidence of vascular invasion and metastatic disease.
- One lesion, up to 6.5 cm in diameter.
Section 2: Prevention
Not applicable for this topic.
Section 3: Diagnosis
Indications for an LT evaluation
- Patients with ESLD with a MELD score ≥15.
- Patients with complications of cirrhosis: ascites, encephalopathy, synthetic dysfunction or variceal bleeding. Prior to 2002, allocation of deceased donor organs was determined largely by the Child–Pugh score. Originally used to assess the risk of mortality in cirrhotic patients undergoing surgery, this score was subsequently used to determine their need to undergo LT.
- The Child–Pugh score utilizes five variables: total bilirubin, albumin, prothrombin time, degree of ascites and hepatic encephalopathy.
- Each variable is assigned 1, 2 or 3 points depending on severity, making a maximum score of 15 points.
- The Child–Pugh score utilizes five variables: total bilirubin, albumin, prothrombin time, degree of ascites and hepatic encephalopathy.
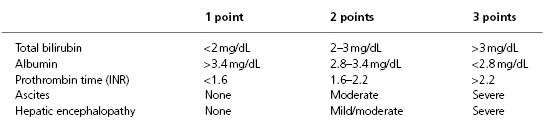
- Categories (Child Class A, B, C) are assigned according to the score range:
- Child Class A: 5–6 points
- Child Class B: 7–9 points
- Child Class C: 10–15 points
- Child Class A: 5–6 points
- A patient needed to be at least Child Class B for LT candidacy consideration (prior to the current use of the MELD score for organ allocation).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


