Hernias in Adults
Epigastric hernias
Epigastric hernias occur in the midline of the abdominal wall between the umbilicus and the xiphoid in a small area of congenital weakness of the linea alba that may contain incarcerated preperitoneal fat. Multiple hernias are reported in 20% of cases.
Clinical presentation, diagnosis investigation, and management
Although most epigastric hernias are asymptomatic, some produce symptoms ranging from a small, painless nodule to acute obstruction of the small intestine. Pain that is exacerbated by exertion and relieved by reclining is characteristic. Raising the head from the examining table may increase pain. The diagnosis, which may be difficult in obese patients with small hernias, is made by palpation of a tender mass on physical examination. Surgery is indicated for epigastric hernias.
Umbilical hernias
Umbilical hernias in adults occur in multiparous women, obese individuals, and up to 40% of cirrhotic patients with ascites. Intestinal or omental incarceration and strangulation complicate 20–30% of cases, especially if the umbilical ring is small. Other complications in cirrhotic patients with ascites are hernia ulceration and perforation, which may be further complicated by peritonitis (often caused by Staphylococcus aureus) or renal failure.
Clinical presentation, diagnosis investigation, and management
Large umbilical hernias are obvious from physical examination. If the diagnosis is not self-evident, abdominal radiographs may demonstrate an intestinal loop outside the abdominal wall. Umbilical hernias are treated surgically. Preoperative control of ascites is important to avoid failure of the repair.
Groin hernias
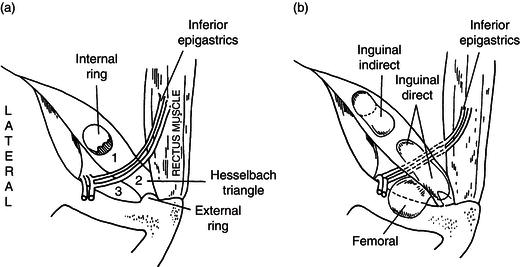
Groin hernias represent 85% of all hernias (Table 36.1). There are three clinically relevant types: indirect inguinal hernias (through the internal inguinal ring into the inguinal canal), direct inguinal hernias (superior to the inguinal ligament but not through the inguinal canal), and femoral hernias (inferior to the inguinal ligament and medial to the epigastric vessels) (Figure 36.2). Most inguinal hernias occur in males, with a male-to-female ratio of about 7/1, whereas there is a female predominance by 2/1 in the incidence of femoral, umbilical, and incisional hernias. Although femoral hernias are more common in women than in men, indirect inguinal hernias are the most common hernias in women. Most groin hernias contain ileum, omentum, colon, or bladder. An indirect inguinal hernia containing a Meckel diverticulum is known as a Littre hernia. Inguinal hernias are thought to originate from a patent processus vaginalis in conjunction with conditions associated with increased intra-abdominal pressure such as chronic cough, pregnancy, massive ascites, and extreme athletics.
Table 36.1 Epidemiology of groin hernias*
| Hernia type | Occurrence (%) |
| Inguinal | 80 |
| Indirect | (48) |
| Direct | (24) |
| Both | (8) |
| Femoral | 5 |
| Inguinal and femoral | 2 |
| With a sliding component | 12 |
| Sigmoid | (8) |
| Cecum | (4) |
| Other | 2 |
*Groin hernias account for 85% of all hernias.
Figure 36.2 The right inguinal region. (a) Schematic anatomy showing internal and external rings and Hesselbach triangle. Spaces where hernias occur include Hesselbach triangle (2), the inguinal canal (1, 2), and the femoral space (3). (b) The most common groin hernias are direct and indirect hernias above the inguinal ligament and femoral hernias below the inguinal ligament. (Source: Yamada T et al. (eds) Textbook of Gastroenterology, 5th edn. Oxford: Blackwell Publishing Ltd, 2009.)
Clinical presentation, diagnosis investigation, and management
A patient with a groin hernia presents with an inguinal mass that appears with increased intra-abdominal pressure. Pain usually is mild; local pain or colicky abdominal pain is suggestive of incarceration or strangulation. The diagnosis of hernias of the groin is made on physical examination by inserting a finger through the external inguinal ring into the inguinal canal to the internal ring. Indirect hernias are felt exiting the internal ring at the examiner’s fingertip, whereas direct hernias are palpated laterally along the side of the finger. Femoral hernias are felt below the inguinal ligament in the femoral region. Strangulation affects 5% of indirect hernias, and 20–30% of femoral hernias strangulate, whereas direct hernias rarely develop this complication. Laparoscopy may visualize the site of herniation and the area of bowel that is trapped. Traditional or laparoscopic surgery is indicated for groin hernias.
Pelvic hernias
Pelvic hernias involve bowel herniation through the obturator foramen, the greater or lesser sciatic foramina, or the perineal muscles. Pelvic hernias are rare; obturator hernias are the most prevalent pelvic hernias. Obturator hernias usually contain ileum and are more common in women.
Clinical presentation, diagnosis investigation, and management
Patients with obturator hernia often have a history of transient attacks of acute intestinal obstruction. Diagnosis usually is made at laparotomy because the obturator is not easily palpated in the thigh. On rectal or vaginal examination, however, a soft, tender, anterolateral, fluctuating mass may be palpated. The Howship–Romberg sign (medial thigh pain radiating to the knee or hip) is present in 50% of patients. An abnormal gas shadow in the intestine may be detected on radiographs of the obturator foramen. A computed tomographic (CT) scan may be diagnostic if there is hernia incarceration. Pelvic hernias are treated surgically.
Lumbar hernias
Lumbar hernias are congenital or they are acquired through flank or rib trauma, through iliac crest fracture, or by removal of a fragment of the iliac crest for bone grafting. Lumbar herniation in the posterior abdominal wall may be superior (bounded by the 12th rib, internal oblique, and sacrospinalis) or inferior (bounded by the iliac crest, latissimus dorsi, and external oblique).
Clinical presentation, diagnosis investigation, and management
Lumbar hernias can be asymptomatic or they can produce lumbar pain referred to the back or pelvis. Surgery is indicated because these hernias generally increase in size.
Spigelian hernias
A spigelian hernia is a small protrusion through the external oblique fascia lateral to the rectus abdominis muscle, below the arcuate line of Douglas. Spigelian hernias are rare and usually occur in elderly persons.
Clinical presentation, diagnosis investigation, and management
Patients present with discomfort from straining or coughing. Sensation of a mass may be reported. A gas shadow may be seen on radiographs of the abdominal wall, whereas upper gastrointestinal contrast radiography may demonstrate bowel lumen outside the abdominal cavity. Surgery is mandatory.
Traumatic diaphragmatic hernias
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






