Overall Bottom Line
- Neonatal cholestasis is a condition characterized by the elevation of conjugated bilirubin.
- Infants with cholestasis often depend on the general practitioner for proper diagnosis and appropriate initial investigations, namely a fractionated serum bilirubin with early referral to a pediatric hepatologist.
- The NASPGHAN Cholestasis Guideline Committee has developed a systematic approach to the evaluation of the cholestatic infant.
- Early diagnosis of the etiology of the cholestasis is essential for effective treatment, most importantly in cases of EHBA, metabolic, or infectious liver diseases, and for management of complications of chronic liver disease.
Section 1: Background
Definition of disease
- Cholestasis is not a disease but is a symptom of underlying disease. It is characterized by abnormal bile formation or flow.
- In cholestatic disorders, there is an elevation of conjugated bilirubin with a direct bilirubin >1 mg/dL or >20% of total bilirubin if total bilirubin is >5 mg/dL.
Incidence/prevalence
- Jaundice may be seen in up to 15% of all newborns.
- However, neonatal cholestasis occurs in approximately one in every 2500 infants and must be distinguished from entities causing an unconjugated hyperbilirubinemia, such as physiologic jaundice or breast milk jaundice.
Etiology
- The differential diagnosis of neonatal cholestasis is broad.
- The most common causes are:
- EHBA: 40%.
- Idiopathic neonatal hepatitis: 10–15%.
- Alpha-1 antitrypsin deficiency: 10%.
- Inborn errors of metabolism: 20%.
- Congenital infections: 5%.
- EHBA: 40%.
Pathology/pathogenesis
- The major determinant of bile flow is the enterohepatic circulation of bile acids. Cholestasis results from impaired bile formation by the hepatocyte (with alteration of key hepatobiliary transporter expression) or from obstruction of bile flow through the intra- or extrahepatic biliary tree with resulting decreased bile flow.
- The neonatal liver is more susceptible to developing cholestasis from a variety of disease processes compared with an older child or adult as there is a smaller bile acid pool and immaturity of hepatic bile acid uptake and excretion systems, leading to reduced enterohepatic circulation of bile acid.
Section 2: Prevention
Bottom Line
- No interventions have been demonstrated to prevent the development of neonatal cholestasis.
Screening
- Currently, there is no screening test to predict which infants will develop cholestasis. Conjugated bilirubin measured in plasma of neonates between 6 and 10 days of life was found to be a sensitive and specific marker of neonatal liver disease. However, development of methods to detect conjugated bilirubin in dried blood spots would be needed for large-scale neonatal screening. In the case of EHBA where timely intervention improves outcomes, Taiwan has implemented a universal screening program for biliary atresia by providing parents with a stool color card on discharge after birth and parents return the stool card at 1 month of age. This screening program has led to earlier detection of EHBA and improved surgical outcomes.
Section 3: Diagnosis (Algorithm 36.1)
– – – – – – – – – –
Algorithm 36.1 Diagnostic approach to neonatal cholestasis
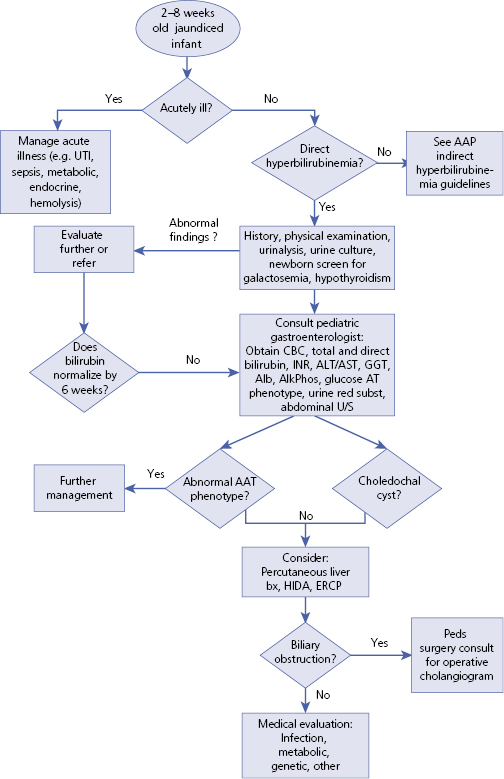
Source: Adapted from Moyer V et al 2004. Reproduced with permission of Wolters Kluwer Health.
– – – – – – – – – –
Bottom Line
- Parents or the primary care physician are the first to recognize signs of cholestasis – jaundice, dark urine or pale colored stools.
- The presentation of a jaundiced infant can reflect either unconjugated or conjugated hyperbilirubinemia – thus formal laboratory testing must be done to test for cholestasis.
- The AAP and NASPGHAN recommend measurement of total and direct serum bilirubin for any infant who is jaundiced at 2 weeks of age. However, breast-fed infants with no history of dark urine or pale stools and normal physical examination who can be reliably monitored may wait until 3 weeks of age to have testing done if jaundice persists at that time.
Differential diagnosis
- First and foremost, it is paramount to distinguish between conjugated and unconjugated hyperbilirubinemia.
- Second, the practitioner must differentiate between physiologic jaundice and pathologic hyperbilirubinemia. The age of the infant and the duration of the abnormal bilirubin level may aid in differentiating the disorders. Pathologic hyperbilirubinemia often occurs during the first 24 hours of life and may be associated with anemia or hepatosplenomegaly, may demonstrate a rapid rise (>5 mg/dL per day), may be prolonged (>7–10 days in a full-term infant), or may present with elevated conjugated bilirubin level (>1 mg/dL or >20% of TSB).
| Differential diagnosis | Features |
|---|---|
| Physiologic jaundice | Transient elevation of bilirubin values during the second or third day of life |
| Breastfeeding jaundice | Within the first 7 days of life; occurs when breast-fed newborn does not receive adequate breast milk intake due to delayed or insufficient milk production or poor feeding by the newborn. Signs/symptoms of dehydration and weight loss with fewer bowel movements (decreased bilirubin excretion from the body) |
| Breast milk jaundice | Breast-fed newborn; TSB >5 mg/dL but with mildly increased levels that do not require intervention. Typically begins after the first 3–5 days of life, peaks within 2 weeks after birth, and normalized over 3–12 weeks |
| Other causes of unconjugated hyperbilirubinemia | Hemolysis, hypothyroidism, rare inherited disorders of bilirubin excretion or conjugation |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


