Overall Bottom Line
- Patients with underlying acute and chronic liver disease are at risk of morbidity and mortality after surgery.
- The magnitude of the risk is related to the severity of liver disease, the type of surgery and the urgency of the surgery.
- The severity of liver disease as measured by the MELD score and the CTP score can be used to risk stratify patients with liver disease undergoing surgery.
- Even in patients with well-preserved liver synthetic function, the presence of significant portal hypertension can lead to adverse outcomes after surgery, particularly if it involves hepatic resection.
- Acute liver failure and acute AH are generally contraindications for any type of surgery.
Section 1: Background
Definition of disease
- Underlying acute and chronic liver disease has a predictable effect on morbidity and mortality after surgery.
- Quantifying this effect is important prior to surgery to ensure an informed decision is made whether to proceed or not.
Disease classification
- Two scoring systems, the CTP and the MELD have been adapted and evaluated to help clinicians determine perioperative morbidity and mortality in patients with liver disease undergoing surgical procedures.
- The type of surgery and anesthesia also influences the outcome with emergency surgery carrying a particularly high mortality.
Incidence/prevalence
- Based on studies in the 1980s it is estimated that up to 10% of patients with advanced liver disease require a surgical procedure in the final 2 years of life.
- The number of hospital discharges for cirrhosis-related illnesses is close to 400 000 annually in the USA and a large number of patients with liver disease will require surgical intervention.
Etiology
- The risks of surgery in liver disease vary according to the severity of liver disease, type of surgery and the urgency of the procedure.
- Although all causes of cirrhosis can lead to higher morbidity and mortality after surgery, AH has an extremely high mortality after surgery.
- Fulminant liver failure and acute hepatitis with jaundice also appear to have prohibitive risk for surgery.
Pathology/pathogenesis
- The pathogenesis of worsening liver function after surgery is unclear but several mechanisms have been postulated.
- The fact that the risk of surgery is dependent on the severity of liver disease and to a lesser extent on the type of surgery suggests that changes induced by anesthesia and medications used during surgery play a major role, perhaps affecting hepatic blood flow.
- Advanced liver disease is typically associated with systemic and splanchnic vasodilation that leads to activation of the sympathetic nervous system in an attempt to maintain arterial perfusion.
- The normal cardiac inotropic and chronotropic response to stress may be decreased in cirrhotic patients and the combination of a hyperdynamic circulation without compensatory mechanisms can lead to hepatic hypoperfusion during surgery. This can be exacerbated by the type of surgery (particularly laparotomy or cardiac surgery), hemorrhage, vasoactive medications and even patient positioning.
- Underlying liver disease can significantly impair the metabolism of anesthetics and certain medications used during surgery such as benzodiazepines and narcotics and can lead to prolonged depression of the CNS precipitating HE.
- Anesthesia can lead to changes in blood flow to the liver that can occur with general or regional anesthesia, meaning the risk of decompensation after surgery is not necessarily reduced even if local or spinal anesthesia is employed.
Predictive/risk factors for decompensation after surgery in cirrhotic patients
- Child’s C.
- MELD score >15.
- Acute liver failure.
- Jaundice (serum bilirubin >11 mg/dL).
- Emergent surgery.
- Cardiac surgery.
- Abdominal surgery.
Section 2: Prevention
Bottom Line
- No intervention has been shown to prevent the development of hepatic decompensation after surgery in patients with significant liver disease.
Screening
- In patients already known to have liver disease or cirrhosis no screening is required but risk stratification is important.
- However, since liver disease can often be asymptomatic it is important to take a thorough history and physical examination in all patients due to undergo surgery.
- The history will provide any risk factors for viral or alcoholic liver disease.
- A full review of medications is important since drug induced liver disease is common.
- Physical examination should concentrate on looking for stigmata of chronic liver disease.
- There is limited utility in looking for underlying liver disease with blood tests unless there is a clinical suspicion.
- An older study demonstrated only 11 of 7620 patients undergoing elective surgery had abnormal liver tests.
- In addition, liver tests can be normal in well-compensated cirrhotics.
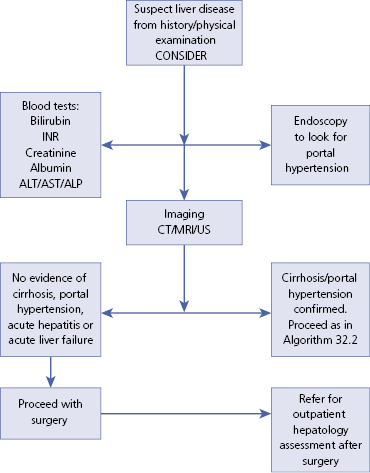
Section 3: Diagnosis (Algorithm 32.1)
– – – – – – – – – –
Algorithm 32.1 Diagnostic algorithm for pre-operative assessment in patients with suspected liver disease
– – – – – – – – – –
Bottom Line/Clinical Pearls
- The history and physical examination remain key in detecting liver disease in patients undergoing surgery.
- In patients with known liver disease, jaundice, prior gastrointestinal bleeding, ascites and encephalopathy in the history may demonstrate evidence of decompensated liver disease.
- In such patients, the physical examination should look for stigmata of chronic liver disease and portal hypertension.
- Laboratory investigations should include a chemistry panel with emphasis on serum bilirubin, albumin, prothrombin time, creatinine and a CBC.
- Abdominal imaging may be required to look for evidence of cirrhosis or portal hypertension.
Typical presentation
- Gastroenterologists or hepatologists are commonly asked to provide a risk assessment before surgery on patients with known liver disease.
- In this situation it is important to determine the severity of liver disease based on the CPT and MELD scores, the type of surgery and anesthesia and the urgency of the surgery.
- Other than deferring surgery in some patients who may have a reversible liver illness, there are no real interventions that can decrease the risk of surgery.
- The primary role of the consultant is to provide an opinion as to the perioperative risk which can then lead to a discussion as to whether to proceed depending on the risk–benefit ratio.
Clinical diagnosis
History
- Patients without a prior history of liver disease should be questioned regarding risk factors such as prior remote blood transfusions, tattoos, illicit drug use, alcohol intake, sexual history, personal history of jaundice, or a family history of liver disease.
- The medication history should include prescription medications but it is important to ask about over-the-counter analgesics and complementary or alternative medications, particularly herbal supplements.
- The review of systems should discuss any excessive fatigue, pruritus and easy bruisability which may be indicators of underlying liver dysfunction.
- In patients with known liver disease the history should concentrate on complaints that might suggest decompensated disease such as:
- Hematemesis, melena or symptoms compatible with gastrointestinal bleeding.
- Abdominal distension and ankle edema.
- Forgetfulness or confusion.
- Hematemesis, melena or symptoms compatible with gastrointestinal bleeding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


