Overall Bottom Line
- HRS is a potentially reversible functional renal insufficiency in patients with cirrhosis, advanced liver failure and portal hypertension.
- There is no specific diagnostic test for HRS. The diagnosis is based on monitoring and interpreting renal function in a patient with liver insufficiency.
- Type 1 HRS is defined by doubling of the initial serum creatinine level to >2.5 mg/dL or 50% reduction of the initial 24-hour creatinine clearance to <20 mL/minute in less than 2 weeks.
- Type 2 HRS is characterized by impairment in renal function leading to serum creatinine level >1.5 mg/dL that does not meet the criteria for type 1 HRS.
- Without appropriate therapy the prognosis is extremely poor with a median survival time from the time of diagnosis of approximately 2 weeks for patients with type 1 HRS and 6 months for patients with type 2 HRS.
- Drug therapy is based on systemic arterial vasoconstrictors combined with volume expansion.
- Liver transplantation is the best treatment option with a 3-year survival rate of approximately 70%.
Section 1: Background
Definition of disease
- HRS is a potentially reversible functional renal insufficiency in patients with cirrhosis, advanced liver failure and portal hypertension in the absence of shock or an intrinsic parenchymal kidney disease.
Epidemiology
- Eighteen percent of patients with decompensated cirrhosis develop HRS within 1 year of decompensation and 39% within 5 years.
- The incidence of HRS in patients with liver cirrhosis who are admitted to the hospital because of ascites formation is 7–15%.
- In acute hepatic failure due to alcoholic hepatitis HRS occurs in approximately 27% of patients.
Etiology
- HRS most often occurs in patients with advanced cirrhosis, but may also complicate acute liver failure.
- Most cases of type 1 HRS are elicited by precipitating factors, such as:
- Infections (SBP is the most common infection precipitating HRS).
- Viral, alcoholic, toxic or ischemic hepatitis superimposed on cirrhosis.
- Major surgical procedures.
- Gastrointestinal bleeding, intensive treatment with diuretics and diarrheal disease may elicit HRS, but more often cause prerenal insufficiency.
- Infections (SBP is the most common infection precipitating HRS).
Pathogenesis
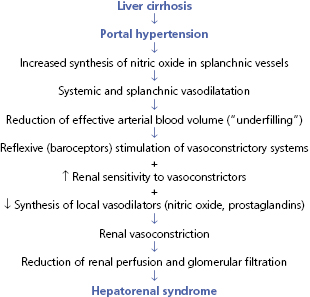
- Changes in endogenous vasoactive systems with marked renal vasoconstriction while at the same time extrarenal arteriolar vasodilatation, decreased systemic resistance and arterial hypotension predominate (Algorithm 22.1).
- The most important pathophysiologic change in HRS is a marked intrarenal arterial vasoconstriction with reduced renal perfusion and reduced glomerular filtration rate.
– – – – – – – – – –
Algorithm 22.1 Pathogenesis of hepatorenal syndrome
– – – – – – – – – –
Predictive factors
- Predictive factors for the development of HRS in non-azotemic patients with liver cirrhosis and ascites:
- Previous episodes of ascites.
- Absence of hepatomegaly.
- Poor nutritional status.
- Moderately reduced glomerular filtration rate (>50 mL/minute).
- Moderately increased BUN (<30 mg/dL).
- Moderately increased serum creatinine (≤1.5 mg/dL).
- Low serum Na+.
- High serum K+.
- Low urinary Na+-excretion.
- Low plasma osmolality.
- High urine osmolality.
- High plasma renin activity.
- Low arterial pressure.
- Reduced free water clearance following a water load.
- Increased plasma norepinephrine.
- Esophageal varices.
- Previous episodes of ascites.
Section 2: Prevention
Screening
- Every patient with liver cirrhosis admitted to the hospital should have serial determinations of serum creatinine levels and/or creatinine clearance.
Prevention
- Avoid and/or eliminate precipitating factors (see “Etiology” in Section 1).
- Patients with spontaneous bacterial peritonitis should be treated with albumin IV since this has been shown to decrease the incidence of HRS and improve survival.
- Pentoxifylline (400 mg PO three times a day for 28 days) has been shown to reduce the incidence of HRS in patients with severe (Maddrey Score >32) alcoholic hepatitis (only one randomized trial).
Section 3: Diagnosis
Clinical Pearls
- There are no specific laboratory tests or imaging methods for the diagnosis of HRS.
- Diagnostic criteria for HRS have been developed by the International Ascites Club (see “Diagnostic criteria (International Ascites Club)”.
- The diagnosis is based on interpreting serial serum creatinine levels and/or creatinine clearance in patients with severe hepatic insufficiency.
- HRS that does not meet the criteria of type 1 HRS is classified as type 2 HRS.
Differential diagnosis
- Most cases of renal dysfunction in cirrhosis are functional in nature. The differential diagnosis encompasses functional circulatory disturbances, obstructive lesions and pre-existing structural changes in the kidneys (acute-on-chronic kidney disease).
- Pre-renal failure:
- volume deficiency (e.g. vomiting, diarrhea, excessive administration of diuretics).
- Acute tubular necrosis:
- circulatory shock, severe bacterial infections, nephrotoxic drugs (NSAIDS, aminoglycosides).
- Post-renal failure
- urinary tract obstruction (e.g. stones, tumors).
- Pre-renal failure:
- Monitoring renal function after withdrawal of diuretic treatment with subsequent intravenous volume expansion allows for important diagnostic conclusions. In pre-renal failure, renal function rapidly improves, while in HRS this measure remains without effect.
Differential diagnostic criteria for kidney dysfunction in cirrhosis
| Diagnosis | Definition |
|---|---|
| Acute kidney injury | Rise in serum creatinine of >50% from baseline or a rise in serum creatinine by ≥26.4 μmol/L (≥0.3 mg/dL) in less than 48 hours HRS type 1 is a specific form of acute kidney injury |
| Chronic renal disease | Estimated glomerular filtration rate of <60 mL/minutes for more than 3 months calculated using the Modification of Diet in Renal Disease 6 (MDRD6) formula HRS type 2 is a specific form of chronic kidney disease |
| Acute-on-chronic kidney disease | Rise in serum creatinine of >50% from baseline or a rise in serum creatinine by ≥26.4 μmol/L (≥0.3 mg/dL) in less than 48 hours in a patient with cirrhosis whose glomerular filtration rate is <60 mL/minute for more than 3 months calculated using the MDRD6 formula |
Differential diagnostic parameters in patients with cirrhosis, ascites and renal insufficiency (serum creatinine >3 mg%)*
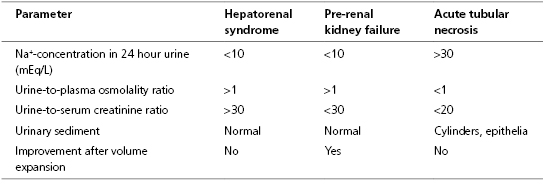
* The parameters traditionally used to differentiate acute tubular necrosis from functional renal failure (urinary sodium excretion and urine: plasma osmolality ratio) are of very limited value in patients with cirrhosis and ascites. Possibly, urinary levels of β2-microglobulin are markers of tubular damage in cirrhosis.
Typical presentation
- The presentation is that of a patient with advanced liver cirrhosis (see Chapter 19).
- Most patients have:
- Diuretic resistant ascites.
- Circulation which is hyperdynamic with high cardiac output and reduced total vascular resistance.
- Diuretic resistant ascites.



