Overall Bottom Line
- HE is a myriad of complex neuropsychiatric symptoms occurring in patients with significant liver dysfunction.
- It occurs most commonly in patients with cirrhosis, but can be a manifestation of ALF or major portosystemic shunts in the absence of cirrhosis.
- HE is an independent predictor of mortality in patients with cirrhosis, with 58% of the patients dying at 1 year and 77% at 3 years.
- The diagnosis of HE is clinical and ammonia levels have limited value except in patient with ALF where it can be a prognostic.
- Treatment of underlying precipitating factors is crucial in the management of HE.
- Lactulose improves symptoms of HE but it is poorly tolerated leading to poor compliance.
- Rifaximin decreases HE-related hospitalizations by 50%.
- Minimal HE is present in 60–80% of patients with cirrhosis and one-third develop overt HE over time.
Section 1: Background
Definition of disease
- HE is a chronically incapacitating syndrome of neuropsychiatric symptoms, which can develop in patients with both acute and chronic liver dysfunction once other known brain diseases have been excluded.
- HE leads to deterioration in mental status, psychomotor dysfunction, impaired memory, increased reaction time, sensory abnormalities, poor concentration, disorientation and in severe forms coma.
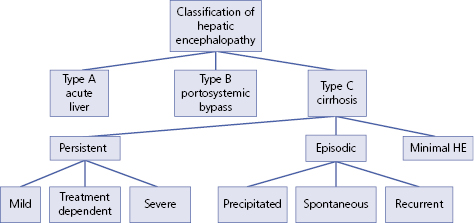
Disease classification (Figure 21.1)
- HE can be classified based on the type of liver dysfunction:
- Type A – acute liver failure.
- Type B – porto-systemic bypass and no intrinsic hepatocellular disease.
- Type C – cirrhosis and portal hypertension.
- Type A – acute liver failure.
- Type C HE can be further classified based on the duration and neurological manifestations:
- Episodic HE: these episodes develop over a short period of time and fluctuate in severity. Episodic HE can be:
- precipitated by an event such as GI hemorrhage or uremia.
- spontaneous, when there is no recognized precipitating factors.
- recurrent encephalopathy, when two episodes of episodic HE occur within 1 year.
- precipitated by an event such as GI hemorrhage or uremia.
- Persistent HE: this includes persistent cognitive deficits that impact negatively on social and occupational functioning of the patient:
- mild (HE grade 1)
- severe (HE grades 2–4)
- mild (HE grade 1)
- MHE: patients with MHE have no recognizable clinical symptoms of HE but do have mild cognitive and psychomotor deficits that are manifested by impairment in specialized testing of cognitive functioning.
- Episodic HE: these episodes develop over a short period of time and fluctuate in severity. Episodic HE can be:
Incidence/prevalence
- Cirrhosis affects about 5.5 million people in the USA and 30–45% of these patients will develop HE.
- HE also develops in 10–50% undergoing TIPS.
Economic impact
- Chronic HE is a common and expensive complication of liver failure, requiring more than 55 000 hospitalizations annually, and costing over $1.2 billion per year in 2003 in the USA alone.
Etiology
- The etiology of HE is primarily due to the accumulation of toxins in the serum due to liver dysfunction.
- The major factors leading to HE are the reduction in the hepatic function and mass accompanied by the development of porto-systemic collaterals which lead to the circulatory bypass of the liver.
- Ammonia is the toxin most frequently implicated in pathogenesis of HE.
Pathology/pathogenesis
- Nitrogenous substances derived from the gut adversely affect brain function. These compounds gain access to the systemic circulation as a result of decreased hepatic function or portal-systemic shunts. Once in brain tissue, they produce alterations of neurotransmission that affect consciousness and behavior, leading to motor dysfunction and extrapyramidal symptoms exhibited in HE.
- The principal neuro-inhibitory neurotransmitter GABA is also increased in the CSF of patients with encephalopathy. Other toxins identified in the CNS include increased levels of endogenous benzodiazepine-like compounds, manganese, oxygen free radicals, circulation opioid peptides and nitric oxide.
Predictive/risk factors
- Increased nitrogen load due GI bleeding, azotemia, infection especially SBP, electrolyte imbalance, blood transfusions, constipation, dehydration and non-compliance with lactulose.
- Decreased toxins clearance due to porto-systemic shunts, spontaneous, surgical, TIPS.
- Altered neurotransmission due to inadvertent use of benzodiazepines or psychoactive drugs.
- Hepatocellular damage with decrease in functional hepatic mass due to continued alcohol abuse, hepatocellular carcinoma or its treatment with TACE and acute portal vein thrombosis.
Section 2: Prevention
Screening
The West Haven Criteria (WHC)
Grade 1
Trivial lack of awareness
Euphoria or anxiety
Shortened attention span
Impaired performance of addition
Grade 2
Lethargy or apathy
Minimal disorientation for time or place
Subtle personality change
Inappropriate behavior
Impaired performance of subtraction
Grade 3
Somnolence to semistupor, responsive to verbal stimuli
Confusion
Gross disorientation
Grade 4
Coma (unresponsive to verbal or noxious stimuli)
Primary prevention
- Pre-emptive use of lactulose after TIPS as one third of patients may develop HE.
- Avoidance of constipation, psychoactive drugs, excessive diuretics.
- Prophylaxis against variceal bleeding and spontaneous bacterial peritonitis that can precipitate HE.
Secondary prevention
- Compliance with lactulose to ensure two to three bowel movements a day.
- Avoidance of sedatives and hypnotics in a hospitalized patient.
- Avoidance of dehydration due to overzealous use of diuretics or lactulose.
- Prompt diagnosis and treatment of GI bleeding or infection.
- Prompt correction of any electrolyte abnormalities.
Section 3: Diagnosis
- The diagnosis of HE is a clinical one based on symptoms reported by patients and more often their caregivers. These include a history of confusion, lethargy, memory loss, disorientation, slowness to respond, personality change with increased aggression or a reversal of day and night sleep pattern.
- In patients with recurrent admissions for HE a history of poor compliance with lactulose or overconsumption of proteins is often elicited.
- In a comatose patient, the presence of clonus may be a sign of HE though it is non-specific.
Differential diagnosis
| Differential diagnosis | Features |
|---|---|
| Metabolic encephalopathies – hypoxia, hyponatremia, azotemia, diabetic coma | Blood gas, clinical chemistry, pulmonary evaluation, urinalysis based on indication |
| Intracranial disorders – tumors, hemorrhage, hematoma, meningitis, seizure disorder, dementia | Neurological imaging, lumbar puncture, EEG based on clinical suspicion, rapid plasma regain, vitamin B12 serum level |
| Toxins – alcohol, drugs, hypnotics, tranquilizers, analgesics, heavy metals | Urine and blood toxin screen, blood alcohol level |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree