Goal: to detect and rule out fluid collection in pericardial space and intra-abdominal cavity
Transducer: 2.5–5.0 MHz sector- or convex-type transducer
Image mode: regular abdomen image mode
Timing of study: during the primary survey for unstable patient or during the secondary survey for stable patient
Pericardial examination: longitudinal or transverse view in the subxiphoid area
Abdominal examination: longitudinal views in right and left upper quadrants, and longitudinal or transverse view of the pelvis
Pericardial Examination
The examination is typically conducted with the ultrasound machine positioned on the patient’s right side, although some perform a FAST from the patient’s left (personal experience, authors). A low-frequency transducer (2.5–5.0 MHz), sector or convex type, is used to maximize penetration. The pericardial examination should be performed prior to the abdominal examination to optimize the ultrasound settings (e.g., gain, depth). The transducer is first oriented in the sagittal plane in the subxiphoid area. The transducer may then be rotated 90° counterclockwise to provide a transverse view of the heart. As the primary goal of FAST is to identify free fluid which appears as an anechoic (dark) space, fluid (blood) inside the atria and ventricles can be used to adjust the settings, particularly the gain to improve image quality (Figs. 8.1 and 8.2). The examination focuses on the identification of free fluid in the pericardial space. Spending extra time to survey for a structural abnormality of the heart during the initial assessment is not necessary and may be harmful if it delays resuscitation or further diagnostic testing. For the patient who is morbidly obese, who has a narrow costal angle, or who has subcutaneous emphysema, the subxiphoid window may be difficult to visualize, and alternate views may need to be acquired.
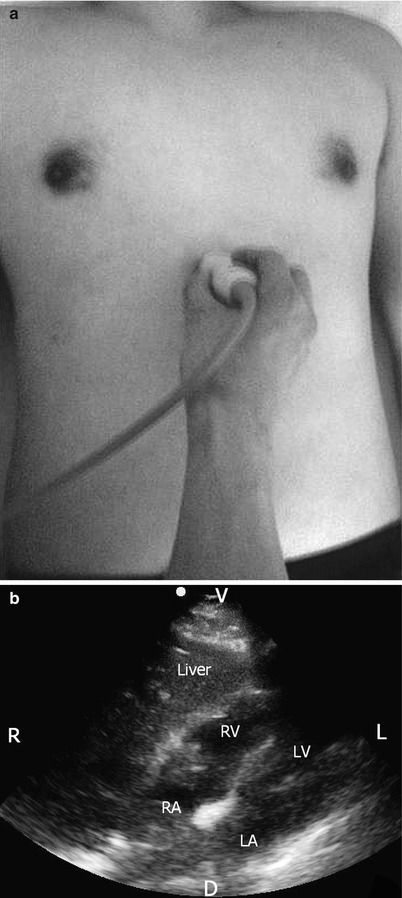
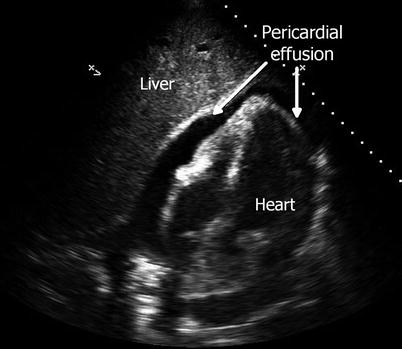
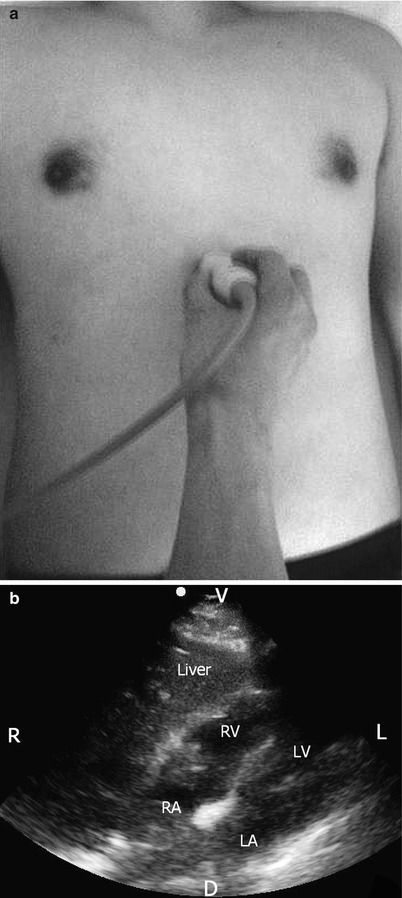
Fig. 8.1
(a, b) Transducer placement for pericardial examination and transverse view of normal pericardial examination with transducer in abdominal preset. RA right atrium, LA left atrium, RV right ventricle, LV left ventricle, R right, L left, V ventral, D dorsal
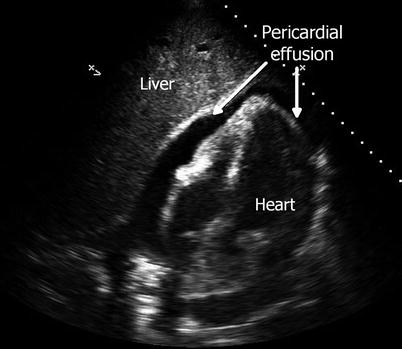
Fig. 8.2
Transverse view of the pericardial examination in an abdominal preset demonstrating a pericardial effusion. Note the small cavity size of the RV. Diastolic collapse of the RV would demonstrate tamponade physiology. RV right ventricle
Abdominal Examination
Next, an examination is performed to survey for free fluid in the abdominal cavity. Three dependent areas are visualized: the hepatorenal recess (Morison’s pouch) in the right upper quadrant, the splenorenal recess in the left upper quadrant, and the pelvic region around the bladder. First, a long-axis view is obtained at the level of 10th to 11th intercostal space in the right mid- to posterior axillary line for surveillance of the hepatorenal recess (Figs. 8.3 and 8.4). Appropriate transducer placement varies based on the patient’s body habitus or history of pulmonary disease. To minimize the false-negative rate, the area of interest should be surveyed entirely by changing the angle of the transducer (fanning). Next, a longitudinal view of the splenorenal recess is obtained in the left upper quadrant (Figs. 8.5 and 8.6). Trauma patients often present with a full stomach that can obscure the penetration of ultrasound. Therefore, transducer placement should be more cephalad and posterior than the analogous view on the right side for better visualization. Finally, the transducer is moved to the pelvis just above the pubic symphysis (Figs. 8.7 and 8.8). The transducer is oriented in either the sagittal or transverse plane.
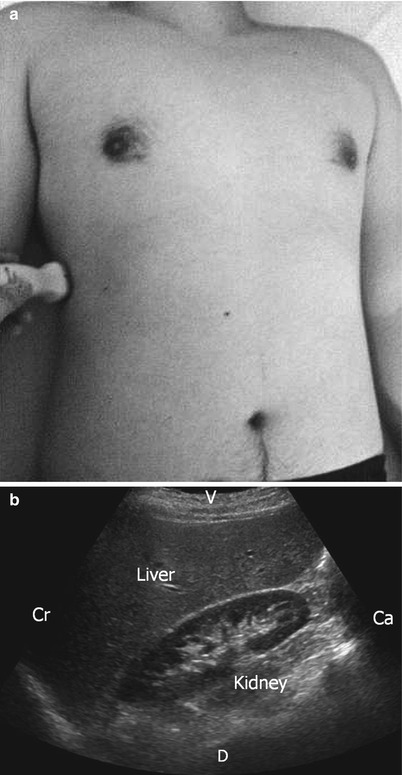
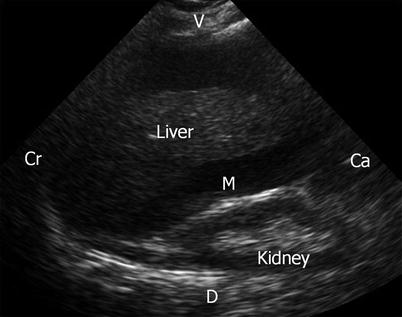
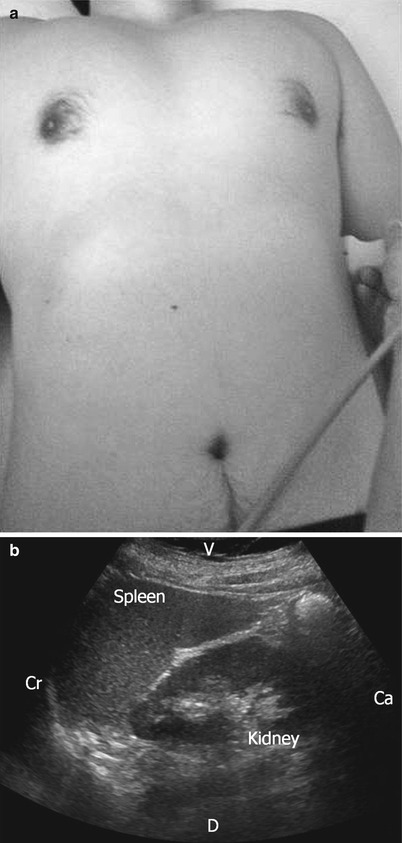
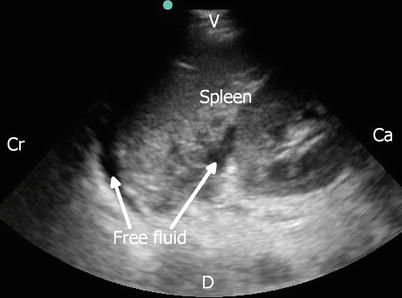
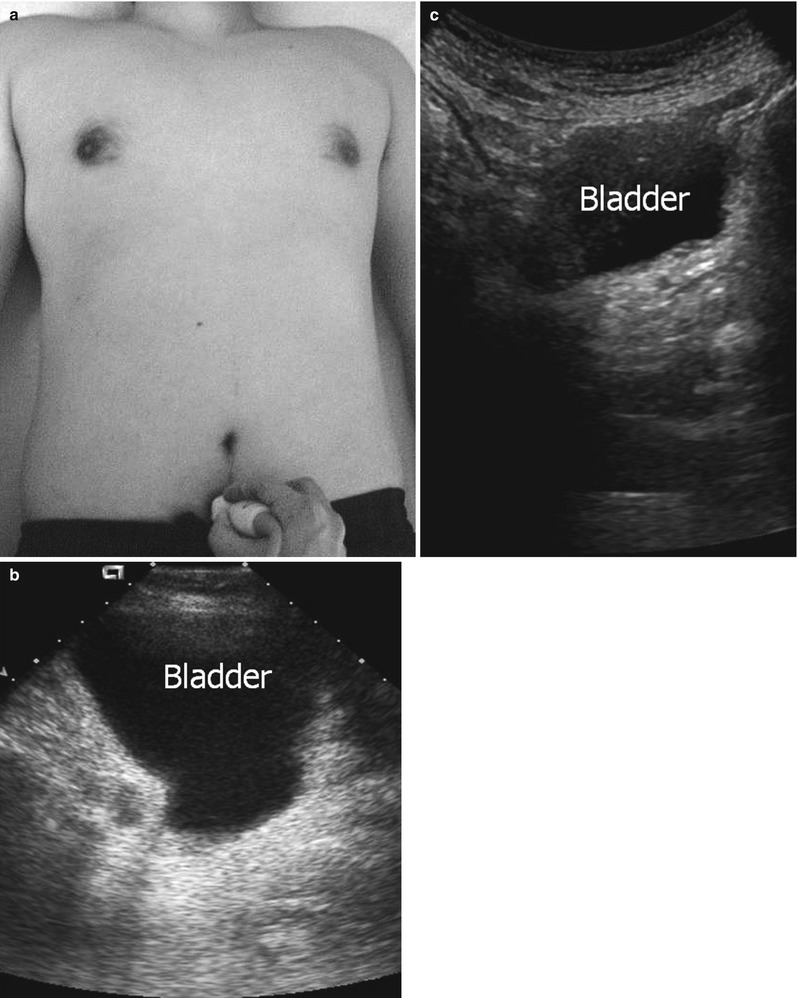
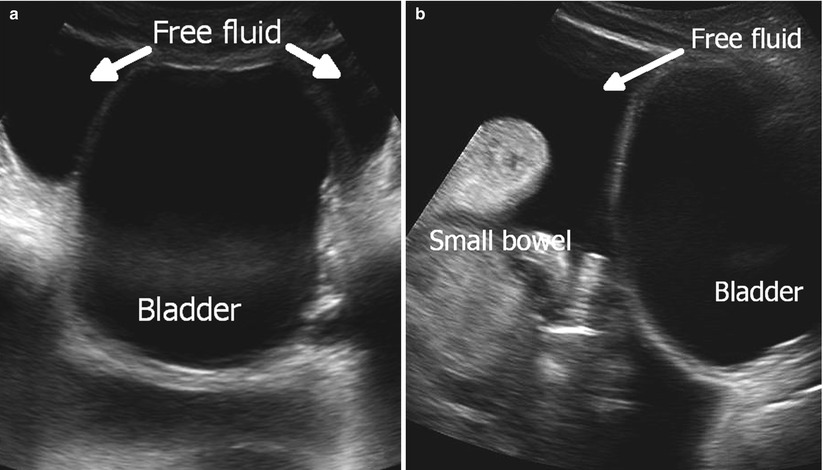
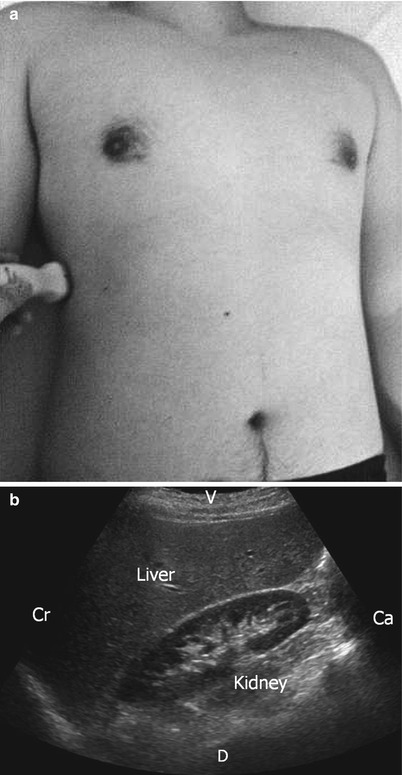
Fig. 8.3
(a, b) Transducer placement for the right upper examination and normal longitudinal view. Cr cranial, Ca caudal, V ventral, D dorsal
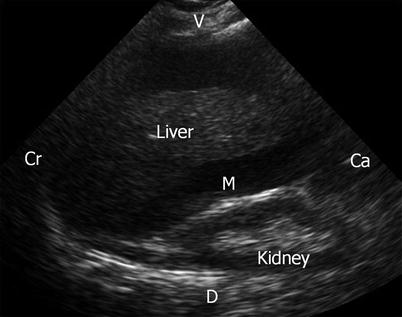
Fig. 8.4
Longitudinal view of the right upper quadrant demonstrating free fluid in Morrison’s pouch and above the liver. Cr cranial, Ca caudal, V ventral, D dorsal, M Morrison’s ouch
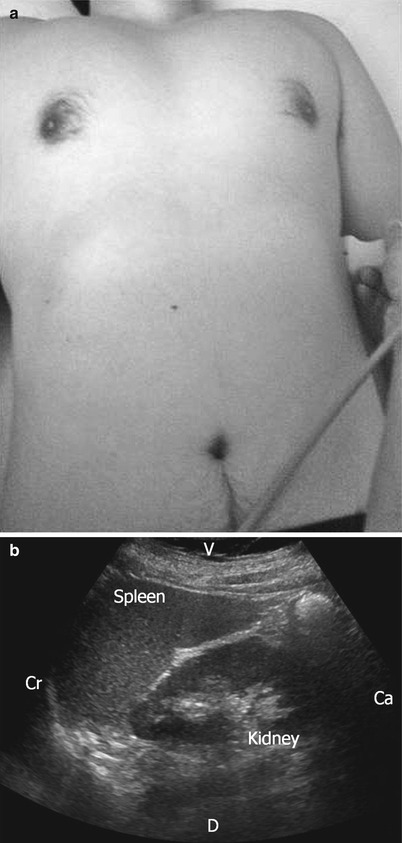
Fig. 8.5
(a, b) Transducer placement for the left upper quadrant and normal longitudinal view. Cr cranial, Ca caudal, V ventral, D dorsal
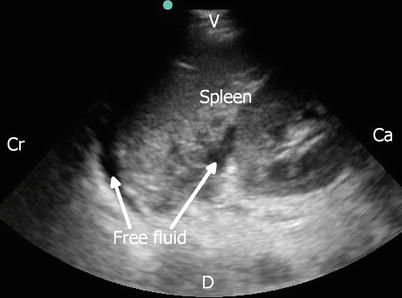
Fig. 8.6
Longitudinal view of the left upper quadrant demonstrating free fluid in the splenorenal recess and above the spleen. Cr cranial, Ca caudal, V ventral, D dorsal
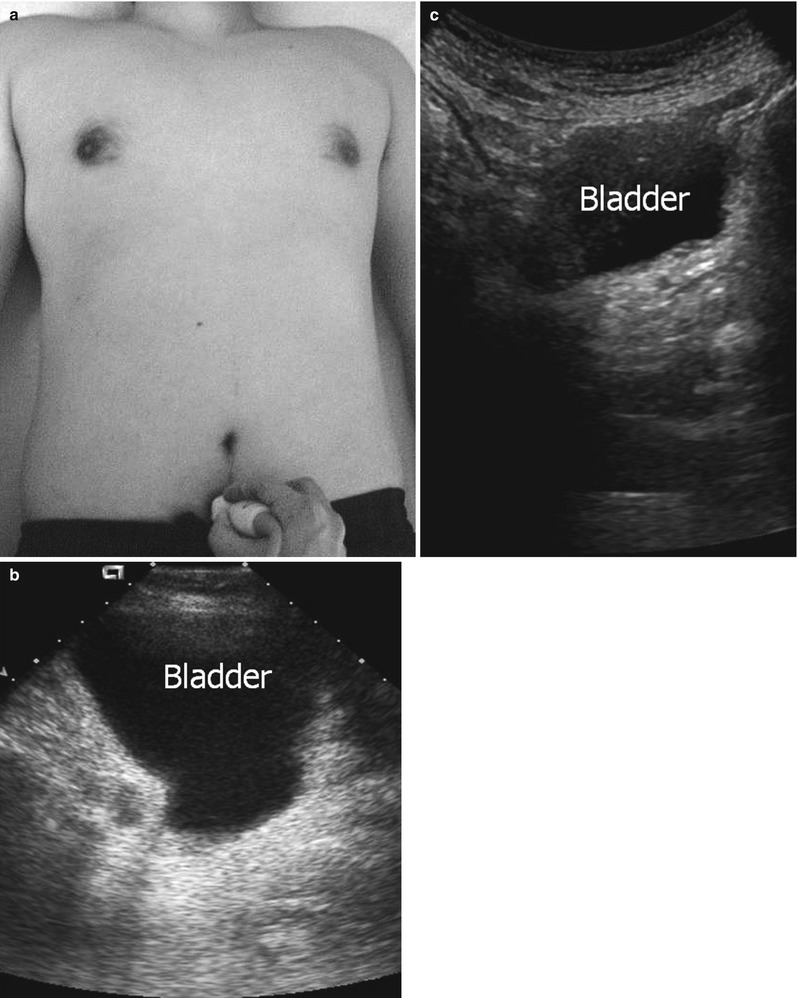
Fig. 8.7
(a–c) Transducer placement for the pelvic view and normal transverse and longitudinal views. (b) Transverse view. (c) Longitudinal view
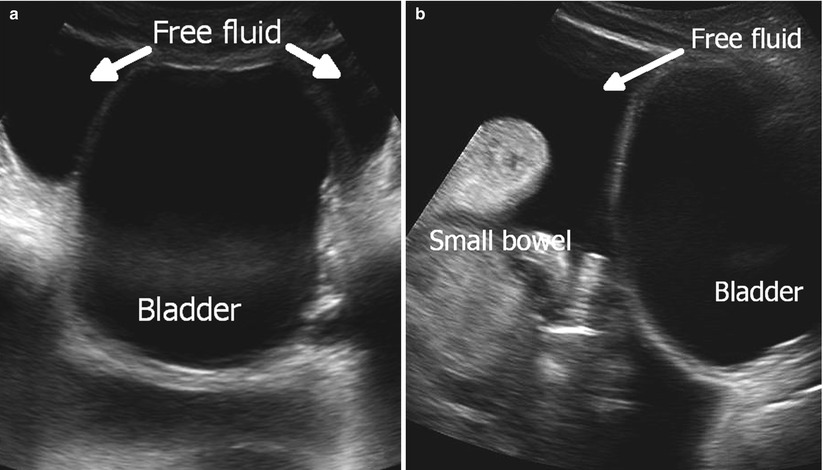
Fig. 8.8
(a, b) Pelvic view demonstrating free fluid. (a) Transverse view. (b) Longitudinal view
FAST: Clinical Data
Blunt Torso Injury
In the United States, the first prospective study of surgeon-performed FAST was conducted by Rozycki and colleagues in 1995 [11]. They showed 78.6 % sensitivity and 100 % specificity for the detection of free fluid among 295 blunt injury patients. Their group reported on a larger number of patients in 1998 [15]. Among 1,227 patients, the sensitivity and specificity was 78.3 and 97.4 %, respectively. While FAST could accomplish a very low false-positive rate, more than 20 % of free fluid was missed according to these data. Friese and associates reported that the sensitivity of FAST was as low as 26 % among the patients with pelvic fractures [16]. Hypotensive patients with positive FAST in the abdomen should be taken to the operating room immediately for exploratory laparotomy. In contrast, intra-abdominal bleeding should not be ruled out just based on a negative or indeterminate FAST in hypotensive patients. These patients need to undergo repeat FAST or an alternate test such as diagnostic peritoneal aspiration (DPA) to confirm the result [17]. However, repeat FAST might not be ideal in the face of continued hemodynamic instability. We also prefer DPA over lavage (DPL) because fluid instilled during the procedure can be confusing on CT images once the patient is stabilized and sent for scanning.
With the development of MDCT, the role of FAST in hemodynamically stable trauma patients is currently of little value (except for triage and education), particularly among the adult population. In addition to a higher sensitivity for intra-abdominal bleeding, the information regarding organ-specific injury can be obtained more accurately by MDCT. In a single-center retrospective study, Natarajan showed that the sensitivity of FAST performed by residents under attending trauma surgeons’ supervision was impressively low (40.8 %). Further, 22 % of false-negative cases required exploratory laparotomy [18]. Additional study will be needed to explore the utility of FAST for stable patients as the risk of radiation exposure by CT to trauma patients is now well recognized [19].
Penetrating Torso Injury
For the patient with penetrating injury to the area known as the “box” or “kill zone” defined as an area bounded by the nipple line bilaterally, sternal notch superiorly, and xiphoid process inferiorly (Fig. 8.9), FAST is a rapid and effective tool for the diagnosis of cardiac injury by detecting pericardial free fluid. From early experience in the 1990s, Rozycki demonstrated that the sensitivity and specificity of FAST approached100 % for the detection of pericardial fluid in the patient with cardiac injury [20]. Of note, in their multicenter study, they showed that FAST could expedite the treatment of cardiac injury (the mean time from a positive pericardial fluid FAST to operation was 12 ± 5 min) [21]. A false-negative FAST is possible in the patient whose pericardial blood decompresses into the chest cavity. The patient usually presents with a large hemothorax with unstable vital signs. Thus, an unstable patient with a “box” injury may need a surgical pericardial window despite a negative FAST. In contrast, epicardial fat pads may be mistaken for pericardial fluid because fat tissue appears as hypoechoic in ultrasound. For the patient in whom visualization of the heart is difficult due to body habitus or injury pattern (wound to the subxiphoid area), an alternate view can be obtained in the second intercostal space (parasternal view) or left nipple area (apical view). Pericardial FAST may also be beneficial to assist in the decision to terminate resuscitative efforts in penetrating (or even blunt) torso trauma, particularly if no injury is visualized in the chest [22, 23].
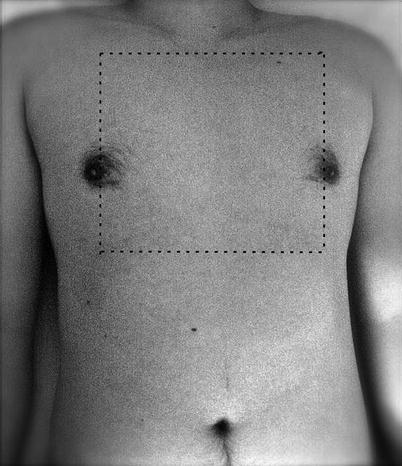
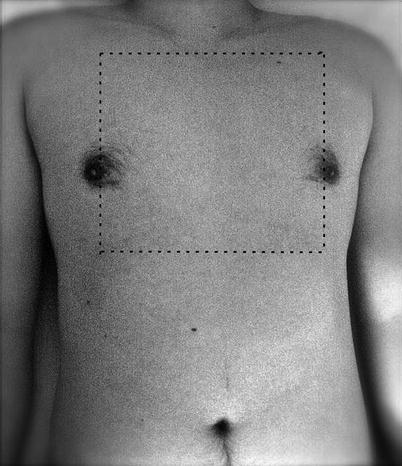
Fig. 8.9
“Box” or “kill zone” demonstrating topographic region where the heart and the great vessels are at risk of injury
In contrast to its use in blunt abdominal injury, FAST is not currently considered the standard imaging modality of choice for penetrating abdominal injury [24]. The accuracy of FAST for penetrating torso injury has been studied since the 1990s [11, 25, 26]. An early study by Rozycki showed that the sensitivity and specificity of FAST for penetrating injury were 83.8 and 97.4 %, respectively [11]. This result is comparable to that for blunt injury. However, a subsequently performed study showed much lower sensitivity, ranging from 46 to 67 % [27]. The biggest reason why FAST is not used for penetrating abdominal injury as often as blunt injury is its low sensitivity for detecting hollow viscus and diaphragm injury that are far more common in penetrating than blunt injury. In other words, a negative FAST cannot safely exclude these injuries. Thus, hemodynamically stable patients with abdominal gunshot or stab wounds with fascial violation may still require exploratory laparotomy to exclude visceral injury that may not be associated with an appreciable amount of free fluid [28]. Soffer demonstrated this low sensitivity of FAST (48 %) in their patients with penetrating injury performed by trauma surgeons and surgical trainees [29]. Not surprisingly, they found a significant number of missed hollow viscus and diaphragm injuries. Likewise, they showed that a positive FAST rarely added any information to change the management of the patient with penetrating torso injury. There were only three patients whose initial management was altered by a positive FAST. All these patients had unclear bullet trajectory with no signs or symptoms for immediate exploration. FAST may be helpful in the situation of the hemodynamically unstable patient with multicavitary penetrating injury to assist in deciding which body cavity to enter first or in the instance of multiple simultaneously penetrating injured patients for triage purposes.
E-FAST: Extended FAST
Principles and Technique
The incidence of pneumothorax or hemothorax is astoundingly common in injured patients [30]. In addition to physical examination during the initial ATLS protocol, chest radiography (CXR) has historically been the diagnostic study of choice to identify these potentially life-threatening injuries. However, the utility of CXR for identifying both pneumothorax and hemothorax is somewhat suspect, with surprisingly low sensitivity, as will be discussed in detail below [31]. For trauma patients, CXR is usually performed with the patient in the supine position to maintain spinal immobilization. As air tends to be loculated anteriorly and fluid (blood) posteriorly, an anterior-posterior view of CXR may not visualize air or blood. For hemodynamically unstable patients with suspected thoracic injury, a so-called normal CXR cannot safely (or often rapidly) exclude the potential for pneumothorax or hemothorax. For example, CXR diagnosis of hemothorax requires the presence of at least 175 mL of fluid in the chest cavity [32]. A recent multicenter study demonstrated that 6 % of patients with occult pneumothoraces (defined as those visualized on CT (or ultrasonography), but not on CXR) eventually required tube thoracostomy due to the progression [33].
E-FAST is performed with the patient in the supine position with the same machine position as with a conventional FAST and starts using a low-frequency transducer (Fig. 8.10). The examination typically adds no more than 2 min to a conventional FAST examination [34]. The initial portion of the E-FAST involves retracing the abdominal right and left upper quadrant views with the transducer oriented in a more cephalad fashion to search for free fluid above the diaphragm. Hemothorax (fluid) is detected as an anechoic (black) area above the diaphragm (Fig. 8.11). Ultrasound can detect as little as 20 mL of fluid in the chest cavity. Clot-bearing hemothoraces might be seen as more hypoechoic (gray). Finally, in patients with moderate to large hemothoraces, the atelectatic (collapsed) lung parenchyma will be a hyperechoic (white) structure floating in the fluid. Also, the thoracic spine can be visualized above the level of diaphragm when the transducer is aimed toward the midline (“spine sign”) as ultrasound penetrates through fluid in the chest cavity. In normal individuals, air in the lung parenchyma obscures the spine in these levels.
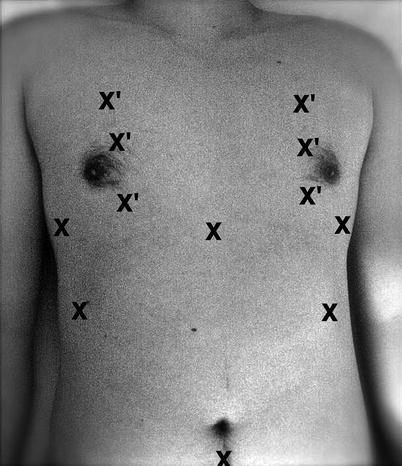
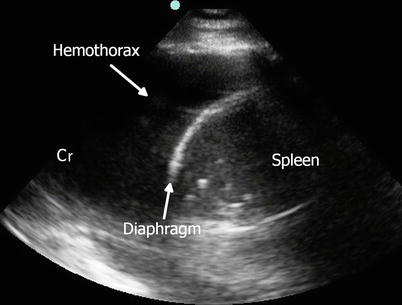
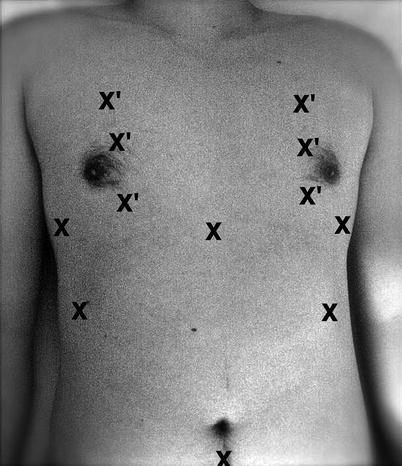
Fig. 8.10
Transducer placement for extended focused assessment with sonography for trauma. X low-frequency transducer, X′ high-frequency transducer
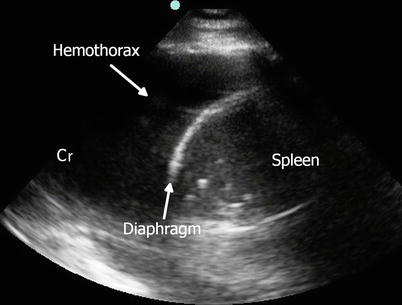
Fig. 8.11
Extended focused assessment with sonography for trauma: free fluid in the thorax (hemothorax) in a longitudinal view of the left upper quadrant with low-frequency transducer directed cranially. Cr Cranial
The remainder of the E-FAST examination is typically performed with a high-frequency (7.5–10 MHz) transducer; however, it can be accomplished with a low-frequency transducer as well. As air is usually located in the anterior chest of a patient in the supine position, the ultrasound images are obtained through the anterior intercostal spaces (high, mid, and low levels) in the midclavicular line bilaterally. The transducer is oriented in the sagittal or long-axis plane. The sonographic finding of a normal lung includes lung sliding and the comet-tail sign (Fig. 8.12). Real-time observation of the parietal and visceral pleura moving in apposition to each other is called “lung sliding” [35]. Comet tails or lung rockets, characterized as vertical, narrow-based, and hyperechoic lines arising from pleural line, represent artifacts resulting from reverberation of ultrasound. Another technique to detect pneumothorax is performed using the M-mode (motion-mode) view as opposed to the B-mode (brightness mode) used in other portions of the E-FAST (see section “Imaging modes”). In the normal lung, a linear pattern of ultrasound image above the pleural line and a granular pattern below the pleural plane are seen, the so-called seashore sign (Fig. 8.12). Pneumothorax can be diagnosed by both the absence of comet tails and of lung sliding. The M-mode view shows loss of the seashore sign, with a similar linear pattern above and below the pleural line, the so-called barcode sign (Fig. 8.13).
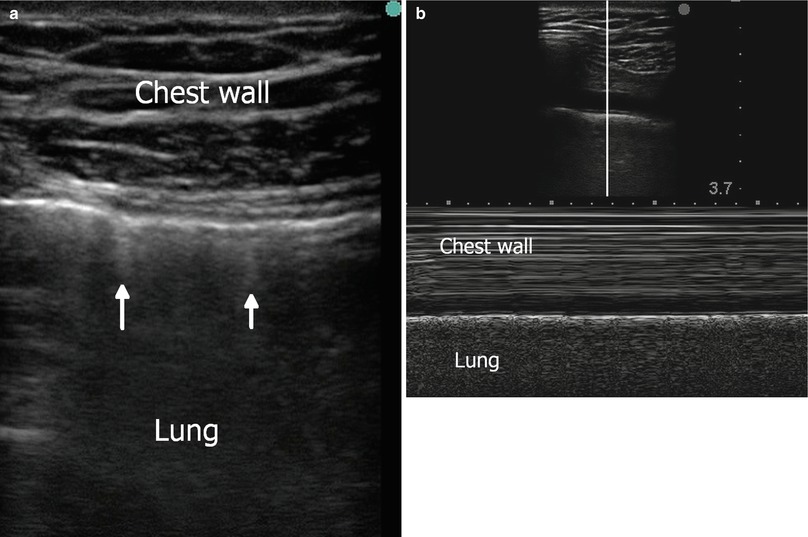
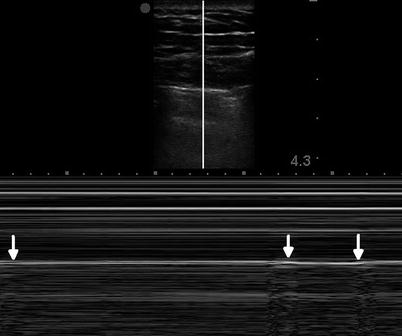
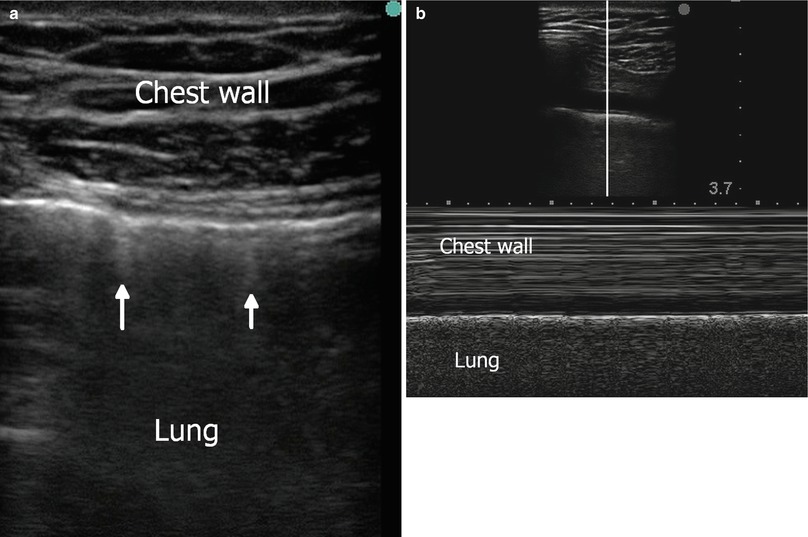
Fig. 8.12
Normal view in thoracic view of extended focused assessment with sonography for trauma using a high-frequency transducer. (a): In B (brightness)-mode view, pleural sliding (see text) and comet-tail sign (arrows) are identified. (b): In M (motion)-mode view, seashore sign (see text) is observed
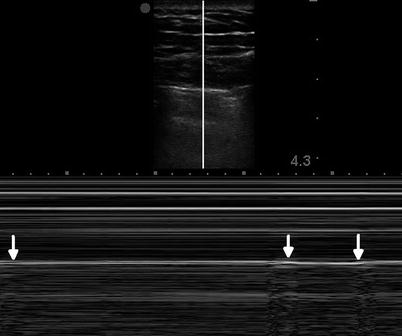
Fig. 8.13
Positive finding (pneumothorax) in thoracic view of extended focused assessment with sonography for trauma using a high-frequency transducer. Loss of seashore sign (barcode sign) is observed. With respiration, normal lung sliding is identified as known as “lung point” (arrows)
Clinical Data
In 1993, Röthlin and colleagues first described, in the English literature, using ultrasound to detect hemothoraces in injured patients [36]. In 1996, Ma and associates conducted a retrospective analysis comparing the sensitivity of ultrasound performed by emergency physicians to CXR for the detection of hemothorax [32]. For 26 patients with hemothoraces, they found a comparable sensitivity and specificity of these imaging modalities (96.2 and 100 %, respectively in both CXR and ultrasound). Sisley and colleagues conducted a prospective study to evaluate the accuracy of surgeon-performed ultrasound for the detection of hemothorax [37]. Again, thoracic ultrasound and CXR had similar sensitivity and specificity (97.5 % sensitivity and 99.7 % specificity for ultrasound and 92.5 % sensitivity and 99.7 % specificity for CXR). Notably, study time for ultrasound was significantly shorter than CXR (1.30 vs. 14.18 min, p < 0.0001). Another prospective study by Brooks documented a high sensitivity of ultrasound for hemothorax [38]. Hyacinthe and colleagues recently reported the diagnostic accuracy of ultrasound compared to clinical examination plus CXR for the detection of thoracic trauma including pneumothorax, hemothorax, and lung contusion [39]. Using CT as a comparison, thoracic ultrasound was superior to clinical examination plus CXR for pneumothorax and lung contusion while similar results were found for hemothorax.
Rantanen and associates described the utility of ultrasound for the diagnosis of pneumothorax in horses in 1986 [40]. Lichtenstein subsequently applied this thoracic ultrasound technique to critically ill patients (using a low-frequency transducer) [35]. The sensitivity and specificity of ultrasound for the detection of pneumothorax were 95.3 and 91.1 %, respectively. Dulchavsky first reported on the accuracy of ultrasound in detecting pneumothorax in injured patients [41]. Compared to CXR, the sensitivity of ultrasound was 95 %. Of note, two pneumothoraces were missed because of concomitant subcutaneous air. Similarly, Knudtson reported 100 % sensitivity and specificity in penetrating trauma and 88.9 % sensitivity and 99.7 % specificity in blunt trauma for ultrasound for the diagnosis of pneumothorax [42]. Subsequently, comparison of the sensitivity between CXR and thoracic ultrasound was performed using CT as a gold standard. Kirkpatrick reported on E-FAST performed by trauma surgeons with a handheld portable ultrasound [34]. The sensitivity of E-FAST for pneumothorax detection was 48.8 %, while the sensitivity of CXR was 20.9 % in 266 patients with CT as a gold standard. A higher sensitivity (>90 %) for thoracic ultrasound in diagnosing pneumothoraces has been observed in more recent studies [43]. A meta-analysis by Alrajhi included eight studies with 1,048 patients [44]. Ultrasound was 90.9 % sensitive and 98.2 % specific for the detection of traumatic or iatrogenic pneumothorax, which was superior to that of CXR (50.2 % sensitivity and 99.4 % specific). In a subgroup analysis of trauma patients, similar results were shown.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







