Obesity is a well-recognized risk factor for gallstone formation and increases the risk for gallstone-related complications. Pancreatic diseases are impacted adversely by obesity. Although weight loss surgery increases the risk of gallstone disease, evidence suggests that bariatric surgery mitigates the obesity-associated adverse prognostication in acute pancreatitis. Obesity is also a significant risk factor for pancreatic cancer. Obesity is a global epidemic and is increasing worldwide and among all age groups. There is an urgent need for focused health policies aimed at reducing the incidence and prevalence of obesity. This article summarizes the current literature highlighting the association between obesity and the pathophysiology and outcome of gallstone disease, pancreatitis, and pancreatic cancer.
Key points
- •
Obesity is frequently associated with gallstone disease, acute pancreatitis, liver steatosis, and gastrointestinal cancers.
- •
The formation of gallstones in patients with obesity is multifactorial. A rapid weight loss in obesity also predisposes patients to gallstone formation.
- •
Obese patients are at increased risk of severe acute pancreatitis. Multiple local and systemic factors contribute to poor outcomes in patients with obesity.
- •
Although recognized as a risk factor for pancreatic cancer, obesity is also associated with poor outcomes after surgery for pancreatic cancer.
Introduction
Obesity is increasing worldwide and the World Health Organization has confirmed this as a global epidemic. Approximately 30% of the world’s population is overweight or obese, and no country has reduced its obesity rates in 33 years. In the United States, approximately 78.6 million (34.9%) of adults are obese, a statistic that has doubled over the past 2 decades. In particular, the prevalence of morbid obesity has rapidly increased with an approximate 70% increment from 2000 to 2010. Furthermore, childhood obesity has more than doubled in children and quadrupled in adolescents in the past 3 decades and this has led to increases in disease rates associated with obesity.
Other than contributing to the metabolic syndrome and cardiorespiratory comorbidities, obesity is frequently associated with gallstone disease, acute pancreatitis, liver steatosis, and gastrointestinal cancers. Gallstone disease is highly prevalent (10%–15% of population) in the Western population and is increasing. In the United States, there were 389,180 hospitalizations in 2012 due to cholelithiasis with cholecystitis. Acute pancreatitis is the most common single gastrointestinal diagnosis for inpatient hospitalization (275,170 hospitalizations in 2012) and costs an estimated 2.6 billion dollars per year in inpatient costs. The prevalence of inpatient hospitalization for acute pancreatitis is increasing annually, which parallels the rising prevalence of obesity. There is an established association between obesity and the development of complications in acute pancreatitis. In addition, obesity increases the risk of developing pancreas cancer in particular, pancreatic ductal adenocarcinoma (PDAC). PDAC is a devastating disease, with a dismal long-term survival. Surgery offers the only possibility of approximating a cure; however, only 20% of patients are eligible because the cancer tends to be detected at a late stage and has already metastasized at diagnosis. In 2016, PDAC became the third leading cause of cancer-related death in the United States and it is projected to become the second by 2030, due to both an aging population and the obesity epidemic.
The aim of this review is to describe the pathophysiology and outcomes of obesity and the association with gallstone disease, acute pancreatitis, and pancreatic cancer.
Introduction
Obesity is increasing worldwide and the World Health Organization has confirmed this as a global epidemic. Approximately 30% of the world’s population is overweight or obese, and no country has reduced its obesity rates in 33 years. In the United States, approximately 78.6 million (34.9%) of adults are obese, a statistic that has doubled over the past 2 decades. In particular, the prevalence of morbid obesity has rapidly increased with an approximate 70% increment from 2000 to 2010. Furthermore, childhood obesity has more than doubled in children and quadrupled in adolescents in the past 3 decades and this has led to increases in disease rates associated with obesity.
Other than contributing to the metabolic syndrome and cardiorespiratory comorbidities, obesity is frequently associated with gallstone disease, acute pancreatitis, liver steatosis, and gastrointestinal cancers. Gallstone disease is highly prevalent (10%–15% of population) in the Western population and is increasing. In the United States, there were 389,180 hospitalizations in 2012 due to cholelithiasis with cholecystitis. Acute pancreatitis is the most common single gastrointestinal diagnosis for inpatient hospitalization (275,170 hospitalizations in 2012) and costs an estimated 2.6 billion dollars per year in inpatient costs. The prevalence of inpatient hospitalization for acute pancreatitis is increasing annually, which parallels the rising prevalence of obesity. There is an established association between obesity and the development of complications in acute pancreatitis. In addition, obesity increases the risk of developing pancreas cancer in particular, pancreatic ductal adenocarcinoma (PDAC). PDAC is a devastating disease, with a dismal long-term survival. Surgery offers the only possibility of approximating a cure; however, only 20% of patients are eligible because the cancer tends to be detected at a late stage and has already metastasized at diagnosis. In 2016, PDAC became the third leading cause of cancer-related death in the United States and it is projected to become the second by 2030, due to both an aging population and the obesity epidemic.
The aim of this review is to describe the pathophysiology and outcomes of obesity and the association with gallstone disease, acute pancreatitis, and pancreatic cancer.
Cholelithiasis and obesity
There are multiple risk factors for gallstones in patients with obesity ( Table 1 ). Although elevated body mass index (BMI) is associated with gallstone disease, a causal association has been demonstrated between increasing BMI and symptomatic gallstones using a mendelian randomization approach. Furthermore, increasing BMI was associated with a 3-fold increment in the risk of cholelithiasis as evidenced in the Nurses’ Health Study involving women between 30 and 55 years of age followed over a total of 18 years. A 2.5-fold increase in risk has also been demonstrated among men between 40 and 55 years of age. As an outcome of obesity-associated gallstone disease, the risk of gallbladder cancer also increases with BMI. The lithogenic mechanisms of obesity are multifold and are depicted in Fig. 1 . These mechanisms can either act alone or contribute in combination. It is of relevance that the presence of components of metabolic syndrome increases the risk of gallstones; a risk of 5% without the presence of metabolic syndrome increases to 25% when all the components are present in a patient.
| Disease or Condition | Pathophysiology | Type of Gallstone |
|---|---|---|
| Pregnancy Oral contraceptives Estrogen therapy |
| Cholesterol |
| Total parental nutrition Octreotide administration Calcineurin inhibitors Fibrates |
| Cholesterol |
| Liver cirrhosis |
| Cholesterol/black pigment |
| Crohn disease Extended ileal resection Cystic fibrosis |
| Cholesterol/black pigment |
| Hemolytic anemia Sickle cell anemia |
| Black pigment |
| Alcohol excess |
| Black pigment |
| Specific ethnic groups (Pima Indians): obesity with diabetes mellitus |
| Cholesterol |
Cholelithiasis after weight loss in obesity
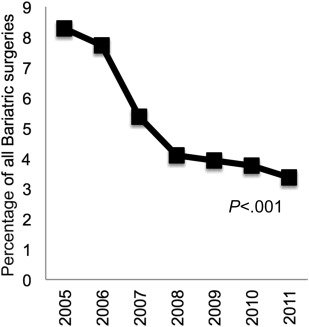
The trend of bariatric surgeries and simultaneous cholecystectomies in the United States (2005–2011) is shown in Fig. 2 . Concomitant cholecystectomy during gastric bypass surgery is no longer the routine practice because the operative time, postoperative hospital stay, and postoperative morbidity and mortality are higher with prophylactic cholecystectomy. Several studies have indicated its use only in cases of symptomatic gallbladder disease, in particular cholelithiasis. Concomitant cholecystectomy (2005–2011) has significantly decreased from 8.3% (9880 of 119,382) to 3.4% (3653 of 108,354) for all types of bariatric surgeries ( P <.001). After bariatric surgery, the incidence of gallstones or sludge is higher compared with the overall population, ranging from 28% to 71%.
Pathogenesis of obesity-associated cholelithiasis
Multiple factors (see Fig. 1 ) may contribute to the increased risk of cholesterol gallstones in obese persons. Because the estimated amount of cholesterol synthesized in the liver is related to body fat, there is increased hepatic secretion of cholesterol in obesity. After this, the bile is saturated with excess cholesterol. Frequently, obese patients have impaired gallbladder motility, which is evident at an early stage of gallstone formation. Due to a combination of these factors, there is aggregation of solid cholesterol crystals and eventual stone formation. This entire process is accelerated in obese patients with weight loss. Other contributing mechanisms include enhanced mobilization of cholesterol, reduced hepatic secretion of biliary bile salts due to decreased hepatic bile acid pool, reduced gallbladder contractility, and increased secretion of biliary calcium.
Management of cholelithiasis
The management of cholelithiasis in obesity is similar to that in the general population. The classic symptoms of upper abdominal pain, which is acute, and characteristic of a biliary colic prompt further investigations. Liver enzymes and an abdominal ultrasound are initial investigations. In the presence of bile duct dilation and/or liver enzyme abnormality, magnetic resonance cholangiopancreatography (MRCP) should be considered if ultrasound has not detected common bile duct stones. If MRCP does not facilitate an accurate diagnosis, then endoscopic ultrasound should be considered. Asymptomatic gallstones with a normal gallbladder and unremarkable-appearing biliary tree do not need further treatment unless patients develop symptoms. Patients with symptomatic gallstones, however, should be offered cholecystectomy and both asymptomatic choledocholithiasis and symptomatic choledocholithiasis require bile duct clearance prior to cholecystectomy.
Although laparoscopic cholecystectomy is the recommended procedure, it is sometimes not possible in morbidly obese patients. The abdominal wall thickness might prohibit maneuverability of trocars requiring longer devices, additional trocars, and procedural modifications to avoid trocar displacement, abdominal wall insufflation, and subcutaneous emphysema. If surgery is prohibitive due to associated comorbidities, oral litholysis with hydrophilic ursodeoxycholic acid (UDCA) can be considered in patients with small (<5 mm), radiolucent gallstones in patients with a patent cystic duct, although there is a higher rate of recurrence of gallstones. Although a majority of weight loss surgeries involve Roux-en-Y gastric bypass (RYGB), the incidence of sleeve gastrectomy has increased in the past 5 years. Despite lower weight loss in sleeve gastrectomy, it has been demonstrated that the incidence of cholecystectomy was similar for both groups of patients at 2-year follow-up after surgery. Rapid weight loss after aggressive diet regimens and gastric by-pass surgery warrants prophylaxis to prevent gallstone formation. The benefit of prophylaxis with oral UDCA has been demonstrated in multiple randomized clinical trials.
Acute pancreatitis and obesity
Prior population-based studies have demonstrated that the incidence of acute pancreatitis in the United States has been increasing. This is true for both emergency department visits and hospital admissions. Despite the increase in incidence, the mortality rate is reportedly lower in the past decade (1% vs 3%–5%). A majority of patients with acute pancreatitis resolve without associated complications. Approximately 20% of patients with acute pancreatitis, however, are severe, with associated local and systemic complications, including pancreatic walled-off necrosis, compartment syndrome, development of acute kidney injury, and acute respiratory distress syndrome. Presence of persistent organ failure constitutes severe acute pancreatitis, which is associated with a higher mortality of approximately 30%.
Several epidemiologic studies suggest obesity or increased intra-abdominal fat is associated with severe acute pancreatitis and morbid obesity is associated with increased in-hospital mortality in acute pancreatitis. Previous single-center studies have revealed correlations between increasing BMI and disease severity, including organ dysfunction, infection, pancreatic necrosis, length of hospital stay, and use of intensive care. Four meta-analyses published within the past 10 years demonstrate that morbid obesity is independently associated with mortality in acute pancreatitis. Most recently, a large Japanese population-based inpatient study demonstrated independent risk of mortality in class 2 and 3 obesity.
Pathogenesis of acute pancreatitis in obesity
Obese patients are at increased risk of severe acute pancreatitis. Multiple local and systemic factors have been implicated in the pathogenesis of adverse prognostication in obesity ( Fig. 3 ). There is evidence of increased pancreatic fat in patients with increasing BMI. It has also been shown that pancreatic fat has a direct toxic effect on the parenchyma of the pancreas. New evidence indicates that fat composition in obesity is predominantly unsaturated and that lipolysis worsens local and systemic injury. The cytokine increase in severe acute pancreatitis is thought to be secondary to lipotoxicity. It has also been demonstrated that deposits of intra-abdominal peripancreatic fat in obese patients undergo necrosis during acute pancreatitis and this contributes to the spectrum of necrotizing pancreatitis. Furthermore, a recent publication demonstrated that peripancreatic fat lipolysis resulted in multisystem injury independent of pancreatic necrosis. Obesity in itself constitutes a low-grade proinflammatory state. A higher level of proinflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-10, IL-6, IL-1β, and plasminogen activator inhibitor-1 have been described. Hence, the inflammatory response is increased and there is an up-regulation of the proinflammatory cytokines that leads to a larger inflammatory response.
In addition to the role of pancreatic and peripancreatic necrosis and inflammatory hypothesis, there is a restriction of chest wall and diaphragmatic movements that leads to decrease in inspiratory capacity and has the net effect of increasing physiologic pulmonary arteriovenous shunting, thus leading to hypoxemia. In acute pancreatitis, hypoxemia produces an oxygen deficit and exacerbates the underlying cellular damage from the inflammatory response, which subsequently increases the rate of multiorgan failure and death.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






