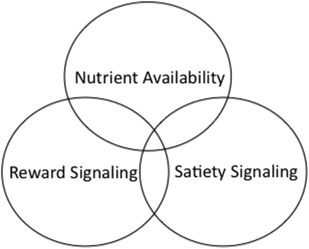
Multiple physiologic and neural systems contribute to the controls over what and how much we eat. These systems include signaling involved in the detection and signaling of nutrient availability, signals arising from consumed nutrients that provide feedback information during a meal to induce satiation, and signals related to the rewarding properties of eating. Each of these has a separate neural representation, but important interactions among these systems are critical to the overall controls of food intake.
Key points
- •
Multiple physiologic and neural systems contribute to the controls over what and how much we eat.
- •
These systems include signaling involved in the detection and signaling of nutrient availability, signals arising from consumed nutrients that provide feedback information during a meal to induce satiation, and signals related to the rewarding properties of eating.
- •
Each of these has a separate neural representation but important interactions among these systems are critical to the overall controls of food intake.
What and how much we choose to eat are influenced by a variety of factors. These include the palatability or taste of particular foods, what we have learned about specific foods through experience, social and cultural influences on what foods and what amounts of food are appropriate to consume, the relative availability and the cost of specific foods, and an interacting system of physiologic controls that serve to both maintain adequate nutrition and limit intake to maximize our use of consumed nutrients. The recent obesity epidemic makes it clear that environmental influences can have a tremendous effect on overall energy balance. Obesity rates began to increase in the United States in the 1970s and this can all be attributed to changes in the food environment. However, the changing food environment interacts with a set of physiologic controls that are important in the meal-to-meal controls of eating.
In this review, we concentrate on the roles of 3 interacting physiologic and neural systems important in feeding control ( Fig. 1 ). These are systems that mediate (1) signals related to metabolic state and nutrient availability, (2) signals that arise during a meal that serve to end that meal and maintain as state of satiety, and (3) affective signals related to taste and nutritional consequences that serve to reinforce aspects of eating. We will also identify how these systems interact in the defense of overall energy balance.
Nutrient availability signaling
Studies of rodent genetic obesity models had long suggested the importance of circulating factors in overall body weight control. Having identified 2 different mutations in mice that led to obesity, led to parabiosis experiments involving 2 strains of obese (obese [ob/ob] and diabetic [db/db]) and normal mice in which the blood supply between 2 mice in a parabiotic pair was shared. The results led to the conclusion that ob/ob mice lacked a circulating satiety factor that, in its absence, results in greatly increased food intake and obesity, whereas the db/db mouse produced the factor but lacked the ability to appropriately respond to that factor. Twenty years later, Friedman and colleagues cloned the ob gene and named the protein that it produced “leptin” from the Greek “leptos” meaning thin, because this was a factor that helped maintain a normal body weight. Shortly thereafter, the leptin receptor protein was identified as the product of the db gene. Leptin is produced primarily in white fat and circulating leptin levels correlate positively with the fat mass, increasing in circulation as animals or humans become obese. Thus, leptin serves as a signal of the available stored energy.
The study of leptin’s actions has illuminated many of the brain circuits that contribute critically to the control of energy balance and provided a basis for understanding earlier lesion work demonstrating a role for hypothalamic nuclei in energy balance. Leptin receptors are expressed throughout the brain with a particularly high expression within hypothalamic nuclei and other brain regions with identified roles in energy balance. Interactions of leptin with its receptors within these hypothalamic nuclei result in the activation or inactivation of hypothalamic pathways containing various peptides that when administered into the brain either stimulate or stop eating.
A major hypothalamic site of leptin’s actions is the arcuate nucleus. The arcuate contains 2 distinct neuronal populations that express leptin receptors. The first are neurons that express the prepropeptide proopiomelanocortin (POMC). POMC is processed into multiple opioid and melanocortin peptides including the anorexigenic peptide α-melanocyte stimulating hormone. Central administration of α-melanocyte stimulating hormone or synthetic melanocortin agonists potently inhibits food intake. Leptin activates POMC neurons, resulting in both increased POMC expression and α-melanocyte stimulating hormone release at terminal sites. Arcuate nucleus POMC expression decreases with food deprivation and increases with overfeeding, suggesting a regulatory role for this peptide in overall feeding control. Important roles for melanocortin signaling in energy balance have been demonstrated in experiments examining the effects of POMC and melanocortin-3 or melanocortin-4 receptor knockouts. Furthermore, genetic mutations in various aspects of the melanocortin signaling pathway have been identified as monogenic causes of human obesity.
Leptin also interacts with arcuate neurons that express the orexigenic peptides, neuropeptide Y (NPY) and the endogenous melanocortin antagonist agouti-related peptide (AgRP). Leptin inhibits neuronal activity in these cells, reducing NPY and AgRP release and downregulates the expression of these peptides. When leptin levels are low, in times of nutrient depletion or food restriction, the leptin inhibitory tone on NPY/AgRP neurons is diminished, activity in these neurons is increased, and the orexigenic peptides NPY and AgRP are released. Lesions of these NPY/AgRP–containing neurons in adulthood results in rapid starvation.
The feeding stimulatory actions of both NPY and AgRP have been well-documented. Intracerebroventricular or direct hypothalamic injection of NPY potently stimulates feeding and repeated or chronic NPY administration results in obesity. Cell bodies of neurons expressing NPY are found in multiple hypothalamic nuclei, including the arcuate and dorsomedial hypothalamic nuclei. Chronic treatment with NPY or viral-induced NPY overexpression can result in obesity.
AgRP is an endogenous melanocortin antagonist whose expression is limited to the NPY/AgRP–expressing neurons within the arcuate nucleus. AgRP expression is upregulated in response to fasting. AgRP or synthetic melanocortin antagonists increase food intake when administered into the brain and their effects are long lasting. GABAergic signaling is an additional important output of NPY/AgRP expressing neurons in their interactions with arcuate POMC neurons exerting an inhibitory tone on anorexigenic signaling and on neurons in the midbrain parabrachial nucleus.
The hypothalamic paraventricular nucleus and the perifornical area of the lateral hypothalamus are important projection sites for arcuate POMC and NPY/AgRP neurons. The paraventricular nucleus contains neuronal populations that mainly express anorexigenic peptides and thus the outputs from this nucleus serve to limit food intake. Leptin and/or melanocortins activate paraventricular nucleus neurons containing corticotrophin releasing factor, oxytocin, and gastrin-releasing peptide and each of these peptides reduce food intake when centrally administered.
The perifornical region of the lateral hypothalamus contains neurons expressing the orexigenic peptides orexin and melanin concentrating hormone (MCH). Preproorexin expression is increased in response to deprivation and decreased in response to leptin administration and central orexin administration increases food intake. Furthermore, administration of an orexin 1 receptor antagonist inhibits eating, suggesting a role for endogenous orexin in food intake control. MCH expressing cells are located similarly in the perifornical region of the lateral hypothalamus, although they represent a distinct neuronal population. MCH expression is increased in response to fasting and is decreased by leptin administration. MCH administration increases food intake in a dose-related fashion and genetic overexpression of MCH results in obesity.
Although leptin is the adiposity signal that has received the most attention, insulin also acts in the hypothalamus as an adiposity signal. Insulin levels increase with increased adiposity, insulin is transported from the circulation into the brain, and insulin receptors are localized to the hypothalamus with a high concentration in the arcuate nucleus. Central insulin administration inhibits food intake and has been shown to modulate activity in the leptin responsive arcuate circuit, decreasing NPY messenger RNA expression and increasing activity in POMC neurons.
Arcuate neurons that respond to leptin and insulin have also been proposed to be responsive to alterations in the local concentrations of nutrients and in this way serve as sensors for both short- and long-term nutrient states. For example, arcuate POMC neurons are activated and NPY/AgRP expressing neurons can be either activated or inhibited by increasing glucose concentration. However, the role of these glucose-induced alterations in electrophysiologic activity in the control of eating is uncertain as brain glucose concentrations do not necessarily reflect changes in circulating glucose or increase in response to meals. Hypothalamic neurons are also responsive to changes in the local concentration of fatty acids and intraventricular administration of a long chain fatty acid has been shown to reduce food intake. These data have been interpreted to suggest a role for brain fatty acid concentrations as signaling nutrient availability. Finally, local hypothalamic administration of some amino acids has been shown to decrease food intake. However, whether such a mechanism is involved in signaling circulating protein availability has yet to be demonstrated.
Although the hypothalamus has been a primary focus of the study of anorexigenic and orexigenic neuropeptide signaling, the neural pathways regulating energy balance are clearly distributed to multiple brain sites. For example, leptin receptors are expressed in the nucleus of the solitary tract (NTS) in the dorsal hindbrain. Local leptin administration at this site reduces food intake and downregulation of NTS leptin receptors attenuates the ability of leptin to reduce food intake. Data such as these strongly support the view that the adiposity controls of food intake are distributed rather than simply localized to the hypothalamic arcuate nucleus.
Satiety signaling
In people and many experimental models for the study of feeding control, eating is not a continuous activity, but occurs in distinct bouts or meals. Meal initiation is determined by a variety of factors, especially food availability. During a meal, ingested nutrients contact a variety of receptors within the oral cavity and gastrointestinal tract resulting in neural and hormonal signals that contribute to the determination of meal size. Meal size can be highly variable and alterations in meal size seem to be a major determinant of overall food intake.
Taste plays a major role in both food choice and in the amount of a particular food that is consumed. The effects of taste on overall ingestion are best demonstrated under conditions in which the feedback from the gastrointestinal tract is minimized. Experimental paradigms that specifically assess the effects of taste or palatability on ingestion have been commonly used. The first of these is called “sham feeding,” in which animals have an esophageal or gastric fistula so that consumed liquid nutrients drain out of the fistula and do not accumulate in the stomach or pass on to the intestine. Such a preparation was first used by Pavlov. Pavlov demonstrated that dogs with open esophageal fistulas did not develop satiety but continued to eat for hours. The sham feeding paradigm has demonstrated the important role of orosensory stimuli in ingestion. Increasing the concentration of sugar solutions or oil emulsions increases the amount consumed in a linear fashion over extensive concentration ranges. Sham feeding does eventually stop and a number of processes have been proposed to contribute to the cessation of sham feeding including oral metering, habituation and sensory-specific satiety (decreasing the pleasantness of a specific food as more is ingested).
In normal ingestion, consumed nutrients contact gastrointestinal mechanosensitive and chemosensitive receptors that provide feedback information that is important to the control of meal size. The potential range of feedback mechanisms that could be operating to lead to meal termination depends on the distribution of ingested nutrients during the meal. During eating, gastric emptying is more rapid than after a meal, meaning that before meal termination, ingested nutrients not only accumulate within the stomach but also come into contact with a significant portion of the small intestine. Thus, the stomach and the upper small intestine are potential sites for the generation of signals providing feedback on the nature and quantity of consumed nutrients.
The vagus nerve (cranial nerve X) is the major neuroanatomic link between the gastrointestinal tract and brain. Vagal afferent fibers with cell bodies in the nodose ganglion innervate the digestive organs and project to the NTS in the dorsal hindbrain with a rough viscerotopic representation of the alimentary canal. The response properties of vagal afferent fibers depend in part on the target organ they innervate. Mechanosensitive gastric vagal afferents increase their firing in response to increasing gastric load volume. Individual afferent fibers are differentially tuned such that there are differences in their dynamic range. Some afferents reach their maximal activity at small intragastric volumes, whereas others do not begin to respond until a significant gastric load is present. Gastric mechanoreceptive vagal afferent fibers do not respond directly to the nutrient character of the gastric contents. Firing rates are similarly increased by nutrient and nonnutrient load volumes. In contrast, duodenal vagal afferents are activated by both the volume and nutrient character of intestinal contents. Although gastric vagal activity is not responsive directly to intragastric nutrient character, gastric afferent responsivity can be altered by the presence of duodenal nutrients.
Alterations in vagal afferent activity may be stimulated by nutrient induced release of a range of gastrointestinal peptides. For example, the brain/gut peptide cholecystokinin (CCK) is released by the duodenal presence of nutrient digestion products. Duodenal vagal afferents that express CCK receptors are activated by local CCK administration and combinations of duodenal load and CCK combine to produce greater duodenal vagal afferent activity than either alone. CCK also plays a role in the response of duodenal vagal afferents to duodenal nutrients. CCK administration results in increases in vagal gastric mechanoreceptive afferent activity similar to those produced by intragastric load and, again, combinations of gastric load and CCK produce greater degrees of activity than either alone. Experiments with CCK receptor antagonists have demonstrated that endogenous CCK plays a role in the response of duodenal afferents to nutrients.
Elimination of aspects of vagal afferent or peptide-induced feedback can result in significant alterations in meal patterns. For example, surgical vagal deafferentation results in the consumption of larger meals than those consumed by sham operated controls. The number of meals consumed during the day is reduced in response to these meal size increases such that overall food intake is unchanged. Similar alterations in meal size also occur in response to the administration of CCK antagonists.
A number of peripherally acting peptides with roles in the control of eating have been identified. The best characterized of these is the brain–gut peptide CCK. CCK is released from I cells in the upper intestine in response to the presence of intraluminal nutrients. Exogenously administered CCK was originally demonstrated to decrease food intake in rats and this feeding inhibitory action of CCK and CCK agonists has been demonstrated in a range of species including nonhuman primates and man. Exogenously administered CCK reduces meal size and results in an earlier appearance of a behavioral satiety sequence. A role for CCK in the control of the size of individual meals was confirmed by experiments examining the effects of repeated, meal-contingent administration of CCK. CCK consistently reduces meal size without producing a significant change in overall daily food intake.
As discussed, CCK activates vagal afferents. Disruption of subdiaphragmatic vagal afferent signaling significantly blunts the ability of CCK to inhibit food intake. A role for endogenous CCK in satiety is supported by data demonstrating that administration of CCK antagonists with specificity for the CCK-1 receptor result in increased food intake. This increase is almost completely accounted for by an increase in the size of their first meal. Alterations in meal patterns are also evident in rats lacking CCK-1 receptors—Otsuka Long Evans Tokushima Fatty (OLETF) rats. OLETF rats are obese and hyperphagic. Characterization of their spontaneous solid or liquid food intake has revealed overall increases in daily food intake that are expressed through significant increases in the size of individual meals with an incomplete compensation in meal number.
Satiety actions for the pancreatic peptides glucagon and amylin have also been demonstrated. Eating rapidly elicits an increase in pancreatic glucagon secretion. Glucagon is cleared rapidly from the circulation by the liver and the liver seems to be the site of glucagon’s satiety action. Hepatic–portal infusion of glucagon at meal onset elicits a dose-related reduction in meal size and the satiety action requires the presence of other forms of ingestional consequences because glucagon does not affect intake during sham feeding. The satiety action of pancreatic glucagon is mediated vagally; transection of the hepatic branch of the vagus blocks glucagon satiety. A role for endogenous glucagon in the control of meal size is supported by data demonstrating the ability of hepatic portal infusions of glucagon antibody to increase meal size.
Amylin is cosecreted with insulin from pancreatic beta cells. Amylin plasma levels increase rapidly with meal onset and remain increased for a significant period of time during and after meals. Exogenously administered amylin inhibits feeding in a dose-dependent and behaviorally specific manner. Amylin’s primary site of action is within the area postrema, a hindbrain structure lacking a blood–brain barrier, although recent work has suggested actions in multiple brain areas to affect food intake. A physiologic role for endogenous amylin in feeding controls is supported by experiments demonstrating increases in food intake in response to administration of amylin antagonists.
Both peptide YY (3-36) [PYY(3-36)] and glucagon-like peptide 1 (GLP-1) are secreted from intestinal L cells in response to the intraluminal presence of nutrients. In contrast with CCK, the secretion of PYY and GLP-1 is maintained after meal termination, suggesting roles for these peptides in feeding control beyond the individual meal. Exogenously administered PYY 3-36 has been shown to inhibit food intake in multiple species including man. The feeding inhibitory actions of PYY are likely mediated through interactions with the inhibitory Y2 receptors on NPY/AgRP neurons. Further supporting a brain site of action, PYY 3-36 administration has been shown to modulate patterns of cortical and hypothalamic neuronal activation in human subjects consistent with its actions in inhibiting food intake. Exogenously administered GLP-1 or long-acting GLP-1 receptor agonists inhibit food intake. Meal-contingent GLP-1 administration leads to earlier meal termination and thus reductions in meal size. Prolonged GLP-1 infusions or administration of long acting GLP-1 analogs reduce overall food intake and do so through reductions in meal size. Examinations of a role for endogenous GLP-1 in the controls of meal size have produced mixed results questioning whether meal stimulated intestinal GLP-1 release is involved in meal termination under normal circmstances. Circulating GLP-1 is degraded rapidly by dipeptidyl peptidase-IV (DPP-IV) making it unlikely that feeding actions of the normally released peptide are mediated through endocrine mechanisms. GLP-1 receptors are expressed in vagal afferent neurons and total subdiaphragmatic or specific afferent vagotomy has been demonstrated to significantly attenuate the satiety effects of intraperitoneally administered GLP-1. Thus, meal released GLP-1 may act on vagal afferent terminals in close approximation to the enteroendocrine L cells to affect food intake.
As well as deriving from the lower intestine, GLP-1 is also expressed in neurons within the NTS. These neurons project extensively throughout the brain including to a variety of hypothalamic and reward sites. Centrally administered GLP-1 inhibits food intake, although the effects are site specific. For example, GLP-1 administered into the amygdala not only reduces food intake, but also induces a conditioned taste aversion, whereas GLP-1 administration to hypothalamic, hindbrain, or reward sites seems to have specific feeding inhibitory actions. Whether gut-released GLP-1 affects feeding through activation of specific brain targets has not been investigated adequately. However, GLP-1 and GLP-1 analogs have been demonstrated to readily cross the blood–brain barrier and, thus, degradation-resistant GLP-1 analogs or the high circulating levels found after bariatric surgery likely access central sites to inhibit food intake.
Unlike these peptides that limit food intake, ghrelin, a brain–gut peptide that is primarily synthesized in the stomach, stimulates food intake after either peripheral or central administration. Ghrelin synthesis and plasma ghrelin levels are increased by food deprivation and reduced by refeeding, and this pattern of release in relation to meals is consistent with a role for ghrelin in meal initiation. Repeated exogenous ghrelin administration can result in obesity and ghrelin antagonists have been shown to reduce food intake, supporting a role for the endogenous peptide in stimulating eating. Arcuate NPY/AgRP–containing neurons express ghrelin receptors and peripheral or central ghrelin administration increases arcuate NPY expression, suggesting a hypothalamic site of action. However, ghrelin has also been shown to increase food intake when administered in the hindbrain, leading to the suggestion that ghrelin’s actions are distributed across multiple brain sites. Knockout of either ghrelin or its receptor protects against a high-fat diet–induced obesity and the double knockout results in mice with a lean phenotype.
As well as being modulated by short-term feeding status, plasma ghrelin levels are affected by long-term energy status or adiposity. Thus, ghrelin levels are lower in obesity and increase in response to weight loss. Together with the short-term effects of ghrelin on arcuate NPY, these data suggest a role for ghrelin that opposes that of leptin on overall arcuate signaling.
Reward signaling
As noted, food choice and the amounts consumed are greatly affected by taste or palatability. The effects of palatability on ingestion have been shown to have both opioid and dopaminergic mediation. Opiate agonists increase, whereas antagonists decrease, eating and these effects on ingestion seem to occur through alterations in palatability. Morphine enhances the intake of preferred over nonpreferred diets and enhances hedonic responses to sweet solutions. In contrast, administration of the opioid antagonist naloxone specifically reduces the intake of a preferred diet while not affecting the intake of a nonpreferred diet in a choice paradigm.
A major site of action for opioids in modulating palatability is the nucleus accumbens (NAc). Microinjections of opioid agonists into the medial shell region of the NAc increase both ingestion and positive responses in taste reactivity tests. Furthermore, in a paradigm in which recently consumed tastes are less preferred, NAc injections of opioid agonists increase and antagonists decrease the consumption of a prefed flavor, again suggesting modulation of palatability.
Dopaminergic mediation of palatability has also been documented. Dopamine agonists increase eating and animals with severe neurotoxin-induced dopamine depletions or dopamine deficient through gene knockout fail to consume food independently. Feeding increases extracellular dopamine within the NAc and the increase is greater with the consumption of a highly palatable food, suggesting a role for mesolimbic dopamine in mediating food reward. Such increases can also be shown in response to sham feeding of sucrose or corn oil demonstrating that taste is a sufficient stimulus for increased NAc dopamine release, suggesting that dopamine plays a critical role in the hedonic processing of orosensory stimuli.
Not only the taste but also the nutrient consequences of ingestion can serve to reinforce dietary choice. This is best demonstrated in experiments that pair a novel noncaloric taste with an intragastric nutrient infusion. Animals come to prefer a taste that has been associated with an intragastric nutrient. Although the phenomenon of flavor conditioning is well-documented, its mediation is not well-understood. Feedback pathways that mediate satiety do not seem to be involved. In contrast with the mediation of palatability, nutrient conditioning does not seem to depend on opioid mediation. However, dopaminergic mediation is required because D1 receptor antagonists block or significantly attenuate the acquisition of preferences to a flavor paired with gastric nutrients and this seems to involve a separate population of dopaminergic neurons from those that encode palatability.
Interactions among signaling systems
Although the controls of eating depend on these seemingly separate systems, an important issue is where and how these systems interact to control meals and overall intake. A number of the clearest demonstrations of interactions involve the adiposity signal leptin. Both peripheral and central leptin administration reduce food intake and leptin’s effects on eating are expressed as reductions in meal size without changing meal frequency. Leptin’s actions in reducing meal size depend in part on interactions with satiety signals. For example, administration of leptin at doses that are subthreshold for inhibiting eating when administered alone, enhance the satiating potential of peripheral CCK or an intragastric nutrient preload. This action of leptin seems to depend on its ability to enhance the NTS neural activation produced feedback satiety signaling. That is, leptin enhances the dorsal hindbrain representation of ascending vagal afferent feedback signals arising from CCK or gastric preload induced gastrointestinal stimulation. Reducing leptin levels through food deprivation or exogenous NPY administration have the opposite result – the satiating potency of CCK is reduced and satiety related NTS activation is inhibited. These actions of leptin may be a downstream consequence of leptin signaling in the arcuate nucleus or directly mediated at hindbrain sites since the NTS contains receptors for both leptin and NPY.
Leptin may also decrease meal size by altering the reinforcing effects of ingestion. Leptin receptors are located on ventral tegmental area (VTA) dopamine neurons as well as on lateral hypothalamic neurotensin neurons that project to the VTA and leptin can regulate the activity of VTA. The outcome of such interactions impacts overall reward signaling. Thus, leptin reduces the rewarding efficacy of electrical brain self stimulation and reduces conditioned place preferences to rewarding foods. In contrast, ghrelin has been demonstrated to enhance the rewarding value of high fat diets as reflected in conditioned preferences. Similar effects on reward pathways have been demonstrated for insulin. Thus, adiposity signals serving as long term regulators of energy balance have multiple actions. Many of these may contribute to the controls food intake in ways that both modulate the negative feedback effects of ingestion while also affecting positive feedback. Together these actions result in the modulation of meal size that, over the long term, contribute to the maintenance of energy balance.
Satiety signals can also affect the efficacy of adiposity signals. For example, CCK has been demonstrated to enhance the ability of leptin to reduce food intake and decrease body weight over the longer term. In addition, the satiety signal amylin alters leptin sensitivity, restoring responsivity to exogenous leptin in diet induced obese animals that are otherwise leptin resistant. Satiety signals can also affect reward processing. As noted above, GLP-1 receptors are found in both the VTA and the NAc and administration of GLP-1 or GLP-1 agonists to these brain areas reduces food intake and does so in ways consistent with reduced reward. Similarly, amylin receptor subunits are expressed in the VTA and amylin administration at this site reduces intake and does so by modulating VTA dopaminergic signaling. Amylin receptors are also expressed in the shell region of the NAc and amylin administration can reverse μ-opioid induced feeding through actions at this site.
Finally, alterations in reward signaling can modulate hypothalamic systems involved in feeding control. Palatable diet intake stimulated by NAc μ-opioid agonist administration depends upon activation of multiple hypothalamic sites and suppression of activity in these sites blocks this feeding. Roles for both orexin and NPY in mediating the effects of NAc μ-opioid induced feeding have been demonstrated.
Summary
There are multiple physiologic and neural systems involved in controlling eating. These systems derive from and control different aspects of ingestive behavior and its consequences. While adiposity, satiety and reward signaling have different primary sites of mediation within the brain, these are interacting systems that together modulate food intake. Some of the currently approved pharmacotherapies aimed at reducing eating and body weight target these signaling systems. For example, liraglutide, the active ingredient in Saxenda is a GLP-1 agonist compound targeting satiety signaling, Contrave contains the opioid antagonist naltrexone, targeting reward signaling and locaserin in Belviq is a serotonin agonist thought to act on POMC neurons that contribute to adiposity responses.
Disclosures: T.H. Moran is a consultant for Healthways and Novo Nordisk. E.E. Ladenheim has nothing to declare.
References
- 1. Coleman D.L.: Effect of parabiosis of obese and diabetes and normal mice. Diabetologia 1973; 9: pp. 194-298
- 2. Zhang Y., Proenca R., Maffei M., et al: Positional cloning of the mouse obese gene and its human homologue. Nature 1994; 372: pp. 425-432
- 3. Tartaglia L.A., Dembski M., Weng X., et al: Identification and expression cloning of a leptin receptor, OB-R. Cell 1995; 83: pp. 1263-1271
- 4. Chua S.C., Chung W.K., Wu-Peng X.S., et al: Phenotypes of mouse diabetes and rat fatty due to mutations in the OB (leptin) receptor. Science 1996; 271: pp. 994-996
- 5. Maffei M., Halaas J., Ravussin E., et al: Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med 1995; 1: pp. 1155-1161
- 6. Elmquist J.K., Bjørbaek C., Ahima R.S., et al: Distributions of leptin receptor mRNA isoforms in the rat brain. J Comp Neurol 1998; 395: pp. 535-547
- 7. Schwartz M.W., Seeley R.J., Campfield L.A., et al: Identification of targets of leptin action in rat hypothalamus. J Clin Invest 1996; 98: pp. 1101-1106
- 8. Elias C.F., Aschkenasi C., Lee C., et al: Leptin differentially regulates NPY and POMC neurons projecting to the lateral hypothalamic area. Neuron 1999; 23: pp. 775-786
- 9. Fan W., Boston B.A., Kesterson R.A., et al: Role of melanocortinergic neurons in feeding and the agouti obesity syndrome. Nature 1997; 385: pp. 165-168
- 10. Thiele T.E., van Dijk G., Yagaloff K.A., et al: Central infusion of melanocortin agonist MTII in rats: assessment of c-Fos expression and taste aversion. Am J Physiol 1998; 274: pp. R248-R254
- 11. Cowley M.A., Smart J.L., Rubinstein M., et al: Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature 2001; 411: pp. 480-484
- 12. Schwartz M.W., Seeley R.J., Woods S.C., et al: Leptin increases hypothalamic pro-opiomelanocortin mRNA expression in the rostral arcuate nucleus. Diabetes 1997; 46: pp. 2119-2123
- 13. Enriori P.J., Evans A.E., Sinnayah P., et al: Diet-induced obesity causes severe but reversible leptin resistance in arcuate melanocortin neurons. Cell Metab 2007; 5: pp. 181-194
- 14. Kim E.M., Welch C.C., Grace M.K., et al: Chronic food restriction and acute food deprivation decrease mRNA levels of opioid peptides in arcuate nucleus. Am J Physiol 1996; 270: pp. R1019-R1024
- 15. Hagan M.M., Rushing P.A., Schwartz M.W., et al: Role of the CNS melanocortin system in the response to overfeeding. J Neurosci 1999; 19: pp. 2362-2367
- 16. Challis B.G., Coll A.P., Yeo G.S., et al: Mice lacking pro-opiomelanocortin are sensitive to high-fat feeding but respond normally to the acute anorectic effects of peptide-YY(3-36). Proc Natl Acad Sci U S A 2004; 101: pp. 4695-4700
- 17. Butler A.A., and Cone R.D.: The melanocortin receptors: lessons from knockout models. Neuropeptides 2002; 36: pp. 77-84
- 18. Farooqi I.S., and O’Rahilly S.: Mutations in ligands and receptors of the leptin-melanocortin pathway that lead to obesity. Nat Clin Pract Endocrinol Metab 2008; 4: pp. 569-577
- 19. Luquet S., Perez F.A., Hnasko T.S., et al: NPY/AgRP neurons are essential for feeding in adult mice but can be ablated in neonates. Science 2005; 310: pp. 683-685
- 20. Levine A.S., and Morley J.E.: Neuropeptide Y: a potent inducer of consummatory behavior in rats. Peptides 1984; 5: pp. 1025-1029
- 21. Clark J., Kalra P.S., Crowley W.R., et al: Neuropeptide Y and human pancreatic polypeptide stimulate feeding behavior in rats. Endocrinology 1984; 115: pp. 427-429
- 22. Stanley B.G., Magdalin W., Seirafi A., et al: The perifornical area: the major focus of (a) patchily distributed hypothalamic neuropeptide Y-sensitive feeding system(s). Brain Res 1993; 604: pp. 304-317
- 23. Stanley B.G., Daniel D.R., Chin A.S., et al: Paraventricular nucleus injections of peptide YY and neuropeptide Y preferentially enhance carbohydrate ingestion. Peptides 1985; 6: pp. 1205-1211
- 24. Gehlert D.R., Chronwall B.M., Schafer M.P., et al: Localization of neuropeptide Y messenger ribonucleic acid in rat and mouse brain by in situ hybridization. Synapse 1987; 1: pp. 25-31
- 25. Tiesjema B., la Fleur S.E., Luijendijk M.C., et al: Sustained NPY overexpression in the PVN results in obesity via temporarily increasing food intake. Obesity (Silver Spring) 2009; 17: pp. 1448-1450
- 26. Yang L., Scott K.A., Hyun J., et al: Role of dorsomedial hypothalamic neuropeptide Y in modulating food intake and energy balance. J Neurosci 2009; 29: pp. 179-190
- 27. Hahn T.M., Breininger J.F., Baskin D.G., et al: Coexpression of Agrp and NPY in fasting-activated hypothalamic neurons. Nat Neurosci 1998; 1: pp. 271-272
- 28. Grill H.J., Ginsberg A.B., Seeley R.J., et al: Brainstem application of melanocortin receptor ligands produces long-lasting effects on feeding and body weight. J Neurosci 1998; 18: pp. 10128-10135
- 29. Wu Q., Boyle M.P., and Palmiter R.D.: Loss of GABAergic signaling by AgRP neurons to the parabrachial nucleus leads to starvation. Cell 2009; 137: pp. 1225-1234
- 30. van Dijk G., Seeley R.J., Thiele T.E., et al: Metabolic, gastrointestinal, and CNS neuropeptide effects of brain leptin administration in the rat. Am J Physiol 1999; 276: pp. R1425-R1433
- 31. Masaki T., Yoshimichi G., Chiba S., et al: Corticotropin-releasing hormone-mediated pathway of leptin to regulate feeding, adiposity, and uncoupling protein expression in mice. Endocrinology 2003; 144: pp. 3547-3554
- 32. Lu X.Y., Barsh G.S., Akil H., et al: Interaction between alpha-melanocyte-stimulating hormone and corticotropin-releasing hormone in the regulation of feeding and hypothalamo-pituitary-adrenal responses. J Neurosci 2003; 23: pp. 7863-7872
- 33. Blevins J.E., Schwartz M.W., and Baskin D.G.: Evidence that paraventricular nucleus oxytocin neurons link hypothalamic leptin action to caudal brainstem nuclei controlling meal size. Am J Physiol Regul Integr Comp Physiol 2004; 287: pp. R87-R96
- 34. Ladenheim E.E., Behles R.R., Bi S., et al: Gastrin-releasing peptide messenger ribonucleic acid expression in the hypothalamic paraventricular nucleus is altered by melanocortin receptor stimulation and food deprivation. Endocrinology 2009; 150: pp. 672-678
- 35. Levine A.S., Rogers B., Kneip J., et al: Effect of centrally administered corticotropin releasing factor (CRF) on multiple feeding paradigms. Neuropharmacology 1983; 22: pp. 337-339
- 36. Ladenheim E.E., Taylor J.E., Coy D.H., et al: Hindbrain GRP receptor blockade antagonizes feeding suppression by peripherally administered GRP. Am J Physiol 1996; 271: pp. R180-R184
- 37. Arletti R., Benelli A., and Bertolini A.: Influence of oxytocin on feeding behavior in the rat. Peptides 1989; 10: pp. 89-93
- 38. Lopez M., Seoane L., García M.C., et al: Leptin regulation of prepro-orexin and orexin receptor mRNA levels in the hypothalamus. Biochem Biophys Res Commun 2000; 269: pp. 41-45
- 39. Perez-Leighton C.E., Boland K., Teske J.A., et al: Behavioral responses to orexin, orexin receptor gene expression, and spontaneous physical activity contribute to individual sensitivity to obesity. Am J Physiol Endocrinol Metab 2012; 303: pp. E865-E874
- 40. Haynes A.C., Jackson B., Chapman H., et al: A selective orexin-1 receptor antagonist reduces food consumption in male and female rats. Regul Pept 2000; 96: pp. 45-51
- 41. Qu D., Ludwig D.S., Gammeltoft S., et al: A role for melanin-concentrating hormone in the central regulation of feeding behaviour. Nature 1996; 380: pp. 243-247
- 42. Sahu A.: Evidence suggesting that galanin (GAL), melanin-concentrating hormone (MCH), neurotensin (NT), proopiomelanocortin (POMC) and neuropeptide Y (NPY) are targets of leptin signaling in the hypothalamus. Endocrinology 1998; 139: pp. 795-798
- 43. Rossi M., Choi S.J., O’Shea D., et al: Melanin-concentrating hormone acutely stimulates feeding, but chronic administration has no effect on body weight. Endocrinology 1997; 138: pp. 351-355
- 44. Ludwig D.S., Tritos N.A., Mastaitis J.W., et al: Melanin-concentrating hormone overexpression in transgenic mice leads to obesity and insulin resistance. J Clin Invest 2001; 107: pp. 379-386
- 45. Corp E.S., Woods S.C., Porte D., et al: Localization of 125I-insulin binding sites in the rat hypothalamus by quantitative autoradiography. Neurosci Lett 1986; 70: pp. 17-22
- 46. Woods S.C., Lotter E.C., McKay L.D., et al: Chronic intracerebroventricular infusion of insulin reduces food intake and body weight of baboons. Nature 1979; 282: pp. 503-505
- 47. Schwartz M.W., Sipols A.J., Marks J.L., et al: Inhibition of hypothalamic neuropeptide Y gene expression by insulin. Endocrinology 1992; 130: pp. 3608-3616
- 48. Xu A.W., Kaelin C.B., Takeda K., et al: PI3K integrates the action of insulin and leptin on hypothalamic neurons. J Clin Invest 2005; 115: pp. 951-958
- 49. Moran T.H.: Hypothalamic nutrient sensing and energy balance. Forum Nutr 2010; 63: pp. 94-101
- 50. Levin B.E., Dunn-Meynell A.A., and Routh V.H.: Brain glucosensing and the K(ATP) channel. Nat Neurosci 2001; 4: pp. 459-460
- 51. Levin B.: Neuronal glucose sensing: still a physiological orphan. Cell Metab 2007; 6: pp. 252-254
- 52. Dunn-Meynell A.A., Sanders N.M., Compton D., et al: Relationship among brain and blood glucose levels and spontaneous and glucoprivic feeding. J Neurosci 2009; 29: pp. 7015-7022
- 53. Le Foll C., Irani B.G., Magnan C., et al: Characteristics and mechanisms of hypothalamic neuronal fatty acid sensing. Am J Physiol Regul Integr Comp Physiol 2009; 297: pp. R655-R664
- 54. Oomura Y., Nakamura T., Sugimori M., et al: Effect of free fatty acid on the rat lateral hypothalamic neurons. Physiol Behav 1975; 14: pp. 483-486
- 55. Obici S., Feng Z., Morgan K., et al: Central administration of oleic acid inhibits glucose production and food intake. Diabetes 2002; 51: pp. 271-275
- 56. Obici S., and Rossetti L.: Minireview: nutrient sensing and the regulation of insulin action and energy balance. Endocrinology 2003; 144: pp. 5172-5178
- 57. Cota D., Proulx K., Smith K.A., et al: Hypothalamic mTOR signaling regulates food intake. Science 2006; 312: pp. 927-930
- 58. Morrison C.D., Xi X., White C.L., et al: Amino acids inhibit Agrp gene expression via an mTOR-dependent mechanism. Am J Physiol Endocrinol Metab 2007; 293: pp. E165-E171
- 59. Huo L., Maeng L., Bjørbaek C., et al: Leptin and the control of food intake: neurons in the nucleus of the solitary tract are activated by both gastric distension and leptin. Endocrinology 2007; 148: pp. 2189-2197
- 60. Hayes M.R., Skibicka K.P., Bence K.K., et al: Dorsal hindbrain 5′-adenosine monophosphate-activated protein kinase as an intracellular mediator of energy balance. Endocrinology 2009; 150: pp. 2175-2182
- 61. Hayes M.R., Skibicka K.P., Leichner T.M., et al: Endogenous leptin signaling in the caudal nucleus tractus solitarius and area postrema is required for energy balance regulation. Cell Metab 2010; 11: pp. 77-83
- 62. Grill H.J., and Hayes M.R.: The nucleus tractus solitarius: a portal for visceral afferent signal processing, energy status assessment and integration of their combined effects on food intake. Int J Obes (Lond) 2009; 33: pp. S11-S15
- 63. Grill H.J.: Distributed neural control of energy balance: contributions from hindbrain and hypothalamus. Obesity (Silver Spring) 2006; 14: pp. 216S-221S
- 64. Pavlov I.: The work of the digestiver glands. London: Charles Griffin and Co, Ltd, 1910.
- 65. Mook D.: Oral and postingestional determinants of various solutions in rats with esophageal fistulas. J Comp Physiol Psychol 1963; 56: pp. 645-659
- 66. Weingarten H.P., and Watson S.D.: Sham feeding as a procedure for assessing the influence of diet palatability on food intake. Physiol Behav 1982; 28: pp. 401-407
- 67. Grill H.J., and Kaplan J.M.: Sham feeding in intact and chronic decerebrate rats. Am J Physiol 1992; 262: pp. R1070-R1074
- 68. Mook D.: Satiety, specifications and stop rules: feeding as a voluntary act. In Epstein A., and Morrison A.R. (eds): Progress in psychobiology and physiological psychology. New York: Academic Press, 1990. pp. 1-65
- 69. Swithers S.E., and Hall W.G.: Does oral experience terminate ingestion? Appetite 1994; 23: pp. 113-138
- 70. Rolls B.J.: Sensory-specific satiety. Nutr Rev 1986; 44: pp. 93-101
- 71. Kaplan J.M., Spector A.C., and Grill H.J.: Dynamics of gastric emptying during and after stomach fill. Am J Physiol 1992; 263: pp. R813-R819
- 72. Moran T.H., Knipp S., and Schwartz G.J.: Gastric and duodenal features of meals mediate controls of liquid gastric emptying during fill in rhesus monkeys. Am J Physiol 1999; 277: pp. R1282-R1290
- 73. Prechtl J.C., and Powley T.L.: Organization and distribution of the rat subdiaphragmatic vagus and associated paraganglia. J Comp Neurol 1985; 235: pp. 182-195
- 74. Altschuler S.M., Bao X.M., Bieger D., et al: Viscerotopic representation of the upper alimentary tract in the rat: sensory ganglia and nuclei of the solitary and spinal trigeminal tracts. J Comp Neurol 1989; 283: pp. 248-268
- 75. Andrews P.L., Grundy D., and Scratcherd T.: Vagal afferent discharge from mechanoreceptors in different regions of the ferret stomach. J Physiol 1980; 298: pp. 513-524
- 76. Schwartz G.J., McHugh P.R., and Moran T.H.: Gastric loads and cholecystokinin synergistically stimulate rat gastric vagal afferents. Am J Physiol 1993; 265: pp. R872-R876
- 77. Mathis C., Moran T.H., and Schwartz G.J.: Load-sensitive rat gastric vagal afferents encode volume but not gastric nutrients. Am J Physiol 1998; 274: pp. R280-R286
- 78. Eastwood C., Maubach K., Kirkup A.J., et al: The role of endogenous cholecystokinin in the sensory transduction of luminal nutrient signals in the rat jejunum. Neurosci Lett 1998; 254: pp. 145-148
- 79. Randich A., Tyler W.J., Cox J.E., et al: Responses of celiac and cervical vagal afferents to infusions of lipids in the jejunum or ileum of the rat. Am J Physiol Regul Integr Comp Physiol 2000; 278: pp. R34-R43
- 80. Schwartz G.J., and Moran T.H.: Duodenal nutrient exposure elicits nutrient-specific gut motility and vagal afferent signals in rat. Am J Physiol 1998; 274: pp. R1236-R1242
- 81. Moran T.H., Norgren R., Crosby R.J., et al: Central and peripheral vagal transport of cholecystokinin binding sites occurs in afferent fibers. Brain Res 1990; 526: pp. 95-102
- 82. Schwartz G.J., Tougas G., and Moran T.H.: Integration of vagal afferent responses to duodenal loads and exogenous CCK in rats. Peptides 1995; 16: pp. 707-711
- 83. Schwartz G.J., McHugh P.R., and Moran T.H.: Integration of vagal afferent responses to gastric loads and cholecystokinin in rats. Am J Physiol 1991; 261: pp. R64-R69
- 84. Schwartz G.J., Salorio C.F., Skoglund C., et al: Gut vagal afferent lesions increase meal size but do not block gastric preload-induced feeding suppression. Am J Physiol 1999; 276: pp. R1623-R1629
- 85. Moran T.H., Ameglio P.J., Schwartz G.J., et al: Blockade of type A, not type B, CCK receptors attenuates satiety actions of exogenous and endogenous CCK. Am J Physiol 1992; 262: pp. R46-R50
- 86. Moran T.H., Ameglio P.J., Peyton H.J., et al: Blockade of type A, but not type B, CCK receptors postpones satiety in rhesus monkeys. Am J Physiol 1993; 265: pp. R620-R624
- 87. Gibbs J., Young R.C., and Smith G.P.: Cholecystokinin decreases food intake in rats. J Comp Physiol Psychol 1973; 84: pp. 488-495
- 88. Pi-Sunyer X., Kissileff H.R., Thornton J., et al: C-terminal octapeptide of cholecystokinin decreases food intake in obese men. Physiol Behav 1982; 29: pp. 627-630
- 89. Moran T.H., and McHugh P.R.: Cholecystokinin suppresses food intake by inhibiting gastric emptying. Am J Physiol 1982; 242: pp. R491-R497
- 90. Antin J., Giibs J., Jolt J., et al: Cholecystokinin elicits the complete behavioral sequence of satiety in rats. J Comp Physiol Psychol 1975; 89: pp. 784-790
- 91. West D.B., Fey D., and Woods S.C.: Cholecystokinin persistently suppresses meal size but not food intake in free-feeding rats. Am J Physiol 1984; 246: pp. R776-R787
- 92. Smith G., Jerome C., and Norgren R.: Afferent axons in the abdominal vagus mediate the satiety effects of cholecystokinin in rats. Am J Physiol 1985; 249: pp. R638-R641
- 93. Ritter R.C., and Ladenheim E.E.: Capsaicin pretreatment attenuates suppression of food intake by cholecystokinin. Am J Physiol 1985; 248: pp. R501-R504
- 94. Moran T.H., Baldessarini A.R., Salorio C.F., et al: Vagal afferent and efferent contributions to the inhibition of food intake by cholecystokinin. Am J Physiol 1997; 272: pp. R1245-R1251
- 95. Takiguchi S., Takata Y., Funakoshi A., et al: Disrupted cholecystokinin type-A receptor (CCKAR) gene in OLETF rats. Gene 1997; 197: pp. 169-175
- 96. Moran T.H., Katz L.F., Plata-Salaman C.R., et al: Disordered food intake and obesity in rats lacking cholecystokinin A receptors. Am J Physiol 1998; 274: pp. R618-R625
- 97. Langhans W., Pantel K., Müller-Schell W., et al: Hepatic handling of pancreatic glucagon and glucose during meals in rats. Am J Physiol 1984; 247: pp. R827-R832
- 98. Geary N.: Glucagon and the control of meal size. In Smith G. (eds): Satiation: from gut to brain. New York: Oxford University Press, 1998. pp. 164-197
- 99. Geary N., Le Sauter J., and Noh U.: Glucagon acts in the liver to control spontaneous meal size in rats. Am J Physiol 1993; 264: pp. R116-R122
- 100. Geary N., and Smith G.P.: Pancreatic glucagon fails to inhibit sham feeding in the rat. Peptides 1982; 3: pp. 163-166
- 101. Geary N., and Smith G.P.: Selective hepatic vagotomy blocks pancreatic glucagon’s satiety effect. Physiol Behav 1983; 31: pp. 391-394
- 102. Le Sauter J., Noh U., and Geary N.: Hepatic portal infusion of glucagon antibodies increases spontaneous meal size in rats. Am J Physiol 1991; 261: pp. R162-R165
- 103. Lutz T.A., Geary N., Szabady M.M., et al: Amylin decreases meal size in rats. Physiol Behav 1995; 58: pp. 1197-1202
- 104. Lutz T.A., Senn M., Althaus J., et al: Lesion of the area postrema/nucleus of the solitary tract (AP/NTS) attenuates the anorectic effects of amylin and calcitonin gene-related peptide (CGRP) in rats. Peptides 1998; 19: pp. 309-317
- 105. Mietlicki-Baase E.G., and Hayes M.R.: Amylin activates distributed CNS nuclei to control energy balance. Physiol Behav 2014; 136: pp. 39-46
- 106. Rushing P.A., Hagan M.M., Seeley R.J., et al: Inhibition of central amylin signaling increases food intake and body adiposity in rats. Endocrinology 2001; 142: pp. 5035
- 107. Batterham R.L., Cowley M.A., Small C.J., et al: Gut hormone PYY(3-36) physiologically inhibits food intake. Nature 2002; 418: pp. 650-654
- 108. Batterham R.L., Cohen M.A., Ellis S.M., et al: Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med 2003; 349: pp. 941-948
- 109. Moran T.H., Smedh U., Kinzig K.P., et al: Peptide YY (3-36) inhibits gastric emptying and produces acute reductions in food intake in rhesus monkeys. Am J Physiol Regul Integr Comp Physiol 2005; 288: pp. R384-R388
- 110. Keire D.A., Mannon P., Kobayashi M., et al: Primary structures of PYY, [Pro(34)]PYY, and PYY-(3-36) confer different conformations and receptor selectivity. Am J Physiol Gastrointest Liver Physiol 2000; 279: pp. G126-G131
- 111. Batterham R.L., ffytche D.H., Rosenthal J.M., et al: PYY modulation of cortical and hypothalamic brain areas predicts feeding behaviour in humans. Nature 2007; 450: pp. 106-109
- 112. Ruttimann E.B., Arnold M., Hillebrand J.J., et al: Intrameal hepatic portal and intraperitoneal infusions of glucagon-like peptide-1 reduce spontaneous meal size in the rat via different mechanisms. Endocrinology 2009; 150: pp. 1174-1181
- 113. Chelikani P.K., Haver A.C., and Reidelberger R.D.: Intravenous infusion of glucagon-like peptide-1 potently inhibits food intake, sham feeding, and gastric emptying in rats. Am J Physiol Regul Integr Comp Physiol 2005; 288: pp. R1695-R1706
- 114. Scott K.A., and Moran T.H.: The GLP-1 agonist exendin-4 reduces food intake in non-human primates through changes in meal size. Am J Physiol Regul Integr Comp Physiol 2007; 293: pp. R983-R987
- 115. Ruttimann E.B., Arnold M., Geary N., et al: GLP-1 antagonism with exendin (9-39) fails to increase spontaneous meal size in rats. Physiol Behav 2010; 100: pp. 291-296
- 116. Williams D.L., Baskin D.G., and Schwartz M.W.: Evidence that intestinal glucagon-like peptide-1 plays a physiological role in satiety. Endocrinology 2009; 150: pp. 1680-1687
- 117. Kieffer T.J., McIntosh C.H., and Pederson R.A.: Degradation of glucose-dependent insulinotropic polypeptide and truncated glucagon-like peptide 1 in vitro and in vivo by dipeptidyl peptidase IV. Endocrinology 1995; 136: pp. 3585-3596
- 118. Han V.K., Hynes M.A., Jin C., et al: Cellular localization of proglucagon/glucagon-like peptide I messenger RNAs in rat brain. J Neurosci Res 1986; 16: pp. 97-107
- 119. Goke R., Larsen P.J., Mikkelsen J.D., et al: Distribution of GLP-1 binding sites in the rat brain: evidence that exendin-4 is a ligand of brain GLP-1 binding sites. Eur J Neurosci 1995; 7: pp. 2294-2300
- 120. Kinzig K.P., D’Alessio D.A., and Seeley R.J.: The diverse roles of specific GLP-1 receptors in the control of food intake and the response to visceral illness. J Neurosci 2002; 22: pp. 10470-10476
- 121. Kinzig K.P., D’Alessio D.A., Herman J.P., et al: CNS glucagon-like peptide-1 receptors mediate endocrine and anxiety responses to interoceptive and psychogenic stressors. J Neurosci 2003; 23: pp. 6163-6170
- 122. Dossat A.M., Diaz R., Gallo L., et al: Nucleus accumbens GLP-1 receptors influence meal size and palatability. Am J Physiol Endocrinol Metab 2013; 304: pp. E1314-E1320
- 123. Alhadeff A.L., Baird J.P., Swick J.C., et al: Glucagon-like Peptide-1 receptor signaling in the lateral parabrachial nucleus contributes to the control of food intake and motivation to feed. Neuropsychopharmacology 2014; 39: pp. 2233-2243
- 124. Kastin A.J., Akerstrom V., and Pan W.: Interactions of glucagon-like peptide-1 (GLP-1) with the blood-brain barrier. J Mol Neurosci 2002; 18: pp. 7-14
- 125. Kanoski S.E., Fortin S.M., Arnold M., et al: Peripheral and Central GLP-1 Receptor Populations Mediate the Anorectic Effects of Peripherally Administered GLP-1 Receptor Agonists, Liraglutide and Exendin-4. Endocrinology 2011; 152: pp. 3103-3112
- 126. Tschop M., Smiley D.L., and Heiman M.L.: Ghrelin induces adiposity in rodents. Nature 2000; 407: pp. 908-913
- 127. Wren A.M., Small C.J., Ward H.L., et al: The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion. Endocrinology 2000; 141: pp. 4325-4328
- 128. Cummings D.E., Purnell J.Q., Frayo R.S., et al: A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 2001; 50: pp. 1714-1719
- 129. Wren A.M., Small C.J., Abbott C.R., et al: Ghrelin causes hyperphagia and obesity in rats. Diabetes 2001; 50: pp. 2540-2547
- 130. Asakawa A., Inui A., Kaga T., et al: Antagonism of ghrelin receptor reduces food intake and body weight gain in mice. Gut 2003; 52: pp. 947-952
- 131. Zigman J.M., Jones J.E., Lee C.E., et al: Expression of ghrelin receptor mRNA in the rat and the mouse brain. J Comp Neurol 2006; 494: pp. 528-548
- 132. Kinzig K.P., Scott K.A., Hyun J., et al: Lateral ventricular ghrelin and fourth ventricular ghrelin induce similar increases in food intake and patterns of hypothalamic gene expression. Am J Physiol Regul Integr Comp Physiol 2006; 290: pp. R1565-R1569
- 133. Shintani M., Ogawa Y., Ebihara K., et al: Ghrelin, an endogenous growth hormone secretagogue, is a novel orexigenic peptide that antagonizes leptin action through the activation of hypothalamic neuropeptide Y/Y1 receptor pathway. Diabetes 2001; 50: pp. 227-232
- 134. Seoane L.M., López M., Tovar S., et al: Agouti-related peptide, neuropeptide Y, and somatostatin-producing neurons are targets for ghrelin actions in the rat hypothalamus. Endocrinology 2003; 144: pp. 544-551
- 135. Faulconbridge L.F., Cummings D.E., Kaplan J.M., et al: Hyperphagic effects of brainstem ghrelin administration. Diabetes 2003; 52: pp. 2260-2265
- 136. Zigman J.M., Nakano Y., Coppari R., et al: Mice lacking ghrelin receptors resist the development of diet-induced obesity. J Clin Invest 2005; 115: pp. 3564-3572
- 137. Wortley K.E., Anderson K.D., Garcia K., et al: Genetic deletion of ghrelin does not decrease food intake but influences metabolic fuel preference. Proc Natl Acad Sci U S A 2004; 101: pp. 8227-8232
- 138. Pfluger P.T., Kirchner H., Günnel S., et al: Simultaneous deletion of ghrelin and its receptor increases motor activity and energy expenditure. Am J Physiol Gastrointest Liver Physiol 2008; 294: pp. G610-G618
- 139. Cummings D.E., Weigle D.S., Frayo R.S., et al: Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 2002; 346: pp. 1623-1630
- 140. Gosnell B.A., and Krahn D.D.: The effects of continuous morphine infusion on diet selection and body weight. Physiol Behav 1993; 54: pp. 853-859
- 141. Doyle T.G., Berridge K.C., and Gosnell B.A.: Morphine enhances hedonic taste palatability in rats. Pharmacol Biochem Behav 1993; 46: pp. 745-749
- 142. Glass M.J., Grace M., Cleary J.P., et al: Potency of naloxone’s anorectic effect in rats is dependent on diet preference. Am J Physiol 1996; 271: pp. R217-R221
- 143. Pecina S., Smith K.S., and Berridge K.C.: Hedonic hot spots in the brain. Neuroscientist 2006; 12: pp. 500-511
- 144. Pecina S., and Berridge K.C.: Hedonic hot spot in nucleus accumbens shell: where do mu-opioids cause increased hedonic impact of sweetness? J Neurosci 2005; 25: pp. 11777-11786
- 145. Smith K.S., and Berridge K.C.: Opioid limbic circuit for reward: interaction between hedonic hotspots of nucleus accumbens and ventral pallidum. J Neurosci 2007; 27: pp. 1594-1605
- 146. Woolley J.D., Lee B.S., Taha S.A., et al: Nucleus accumbens opioid signaling conditions short-term flavor preferences. Neuroscience 2007; 146: pp. 19-30
- 147. Sills T.L., and Vaccarino F.J.: Facilitation and inhibition of feeding by a single dose of amphetamine: relationship to baseline intake and accumbens cholecystokinin. Psychopharmacology (Berl) 1991; 105: pp. 329-334
- 148. Ungerstedt U.: Adipsia and aphagia after 6-hydroxydopamine induced degeneration of the nigro-striatal dopamine system. Acta Physiol Scand Suppl 1971; 367: pp. 95-122
- 149. Zhou Q.Y., and Palmiter R.D.: Dopamine-deficient mice are severely hypoactive, adipsic, and aphagic. Cell 1995; 83: pp. 1197-1209
- 150. Hernandez L., and Hoebel B.G.: Feeding and hypothalamic stimulation increase dopamine turnover in the accumbens. Physiol Behav 1988; 44: pp. 599-606
- 151. Martel P., and Fantino M.: Mesolimbic dopaminergic system activity as a function of food reward: a microdialysis study. Pharmacol Biochem Behav 1996; 53: pp. 221-226
- 152. Hajnal A., Smith G.P., and Norgren R.: Oral sucrose stimulation increases accumbens dopamine in the rat. Am J Physiol Regul Integr Comp Physiol 2004; 286: pp. R31-R37
- 153. Liang N.C., Hajnal A., and Norgren R.: Sham feeding corn oil increases accumbens dopamine in the rat. Am J Physiol Regul Integr Comp Physiol 2006; 291: pp. R1236-R1239
- 154. Sclafani A., Ackroff K., and Schwartz G.J.: Selective effects of vagal deafferentation and celiac-superior mesenteric ganglionectomy on the reinforcing and satiating action of intestinal nutrients. Physiol Behav 2003; 78: pp. 285-294
- 155. Azzara A.V., Bodnar R.J., Delamater A.R., et al: Naltrexone fails to block the acquisition or expression of a flavor preference conditioned by intragastric carbohydrate infusions. Pharmacol Biochem Behav 2000; 67: pp. 545-557
- 156. Azzara A.V., Bodnar R.J., Delamater A.R., et al: D1 but not D2 dopamine receptor antagonism blocks the acquisition of a flavor preference conditioned by intragastric carbohydrate infusions. Pharmacol Biochem Behav 2001; 68: pp. 709-720
- 157. Bernal S., Miner P., Abayev Y., et al: Role of amygdala dopamine D1 and D2 receptors in the acquisition and expression of fructose-conditioned flavor preferences in rats. Behav Brain Res 2009; 205: pp. 183-190
- 158. de Araujo I.E.: Circuit organization of sugar reinforcement. Physiol Behav 2016; 164: pp. 473-477
- 159. Eckel L.A., Langhans W., Kahler A., et al: Chronic administration of OB protein decreases food intake by selectively reducing meal size in female rats. Am J Physiol 1998; 275: pp. R186-R193
- 160. Kahler A., Geary N., Eckel L., et al: Chronic administration of OB protein decreases food intake by selectively reducing meal size in male rats. Am J Physiol 1998; 275: pp. R180-R185
- 161. Flynn M.C., Scott T.R., Pritchard T.C., et al: Mode of action of OB protein (leptin) on feeding. Am J Physiol 1998; 275: pp. R174-R179
- 162. Barrachina M.D., Martínez V., Wang L., et al: Synergistic interaction between leptin and cholecystokinin to reduce short-term food intake in lean mice. Proc Natl Acad Sci U S A 1997; 94: pp. 10455-10460
- 163. Emond M., Schwartz G.J., Ladenheim E.E., et al: Central leptin modulates behavioral and neural responsivity to CCK. Am J Physiol 1999; 276: pp. R1545-R1549
- 164. Emond M., Ladenheim E.E., Schwartz G.J., et al: Leptin amplifies the feeding inhibition and neural activation arising from a gastric nutrient preload. Physiol Behav 2001; 72: pp. 123-128
- 165. Schwartz G.J., and Moran T.H.: Leptin and neuropeptide y have opposing modulatory effects on nucleus of the solitary tract neurophysiological responses to gastric loads: implications for the control of food intake. Endocrinology 2002; 143: pp. 3779-3784
- 166. McMinn J.E., Sindelar D.K., Havel P.J., et al: Leptin deficiency induced by fasting impairs the satiety response to cholecystokinin. Endocrinology 2000; 141: pp. 4442-4448
- 167. Moran T.H., Aja S., and Ladenheim E.E.: Leptin modulation of peripheral controls of meal size. Physiol Behav 2006; 89: pp. 511-516
- 168. Grill H.J., Schwartz M.W., Kaplan J.M., et al: Evidence that the caudal brainstem is a target for the inhibitory effect of leptin on food intake. Endocrinology 2002; 143: pp. 239-246
- 169. Mahaut S., Dumont Y., Fournier A., et al: Neuropeptide Y receptor subtypes in the dorsal vagal complex under acute feeding adaptation in the adult rat. Neuropeptides 2010; 44: pp. 77-86
- 170. Figlewicz D.P., Evans S.B., Murphy J., et al: Expression of receptors for insulin and leptin in the ventral tegmental area/substantia nigra (VTA/SN) of the rat. Brain Res 2003; 964: pp. 107-115
- 171. Leinninger G.M., Jo Y.H., Leshan R.L., et al: Leptin acts via leptin receptor-expressing lateral hypothalamic neurons to modulate the mesolimbic dopamine system and suppress feeding. Cell Metab 2009; 10: pp. 89-98
- 172. Fulton S., Woodside B., and Shizgal P.: Modulation of brain reward circuitry by leptin. Science 2000; 287: pp. 125-128
- 173. Figlewicz D.P., Bennett J., Evans S.B., et al: Intraventricular insulin and leptin reverse place preference conditioned with high-fat diet in rats. Behav Neurosci 2004; 118: pp. 479-487
- 174. Perello M., Sakata I., Birnbaum S., et al: Ghrelin increases the rewarding value of high-fat diet in an orexin-dependent manner. Biol Psychiatry 2010; 67: pp. 880-886
- 175. Figlewicz D.P.: Adiposity signals and food reward: expanding the CNS roles of insulin and leptin. Am J Physiol Regul Integr Comp Physiol 2003; 284: pp. R882-R892
- 176. Matson C.A., Reid D.F., Cannon T.A., et al: Cholecystokinin and leptin act synergistically to reduce body weight. Am J Physiol Regul Integr Comp Physiol 2000; 278: pp. R882-R890
- 177. Matson C.A., Wiater M.F., Kuijper J.L., et al: Synergy between leptin and cholecystokinin (CCK) to control daily caloric intake. Peptides 1997; 18: pp. 1275-1278
- 178. Matson C.A., and Ritter R.C.: Long-term CCK-leptin synergy suggests a role for CCK in the regulation of body weight. Am J Physiol 1999; 276: pp. R1038-R1045
- 179. Trevaskis J.L., Coffey T., Cole R., et al: Amylin-mediated restoration of leptin responsiveness in diet-induced obesity: magnitude and mechanisms. Endocrinology 2008; 149: pp. 5679-5687
- 180. Roth J.D., Roland B.L., Cole R.L., et al: Leptin responsiveness restored by amylin agonism in diet-induced obesity: evidence from nonclinical and clinical studies. Proc Natl Acad Sci U S A 2008; 105: pp. 7257-7262
- 181. Alhadeff A.L., Rupprecht L.E., and Hayes M.R.: GLP-1 neurons in the nucleus of the solitary tract project directly to the ventral tegmental area and nucleus accumbens to control for food intake. Endocrinology 2012; 153: pp. 647-658
- 182. Mietlicki-Baase E.G., Reiner D.J., Cone J.J., et al: Amylin modulates the mesolimbic dopamine system to control energy balance. Neuropsychopharmacology 2015; 40: pp. 372-385
- 183. Baisley S.K., and Baldo B.A.: Amylin receptor signaling in the nucleus accumbens negatively modulates mu-opioid-driven feeding. Neuropsychopharmacology 2014; 39: pp. 3009-3017
- 184. Will M.J., Franzblau E.B., and Kelley A.E.: Nucleus accumbens mu-opioids regulate intake of a high-fat diet via activation of a distributed brain network. J Neurosci 2003; 23: pp. 2882-2888
- 185. Zheng H., Patterson L.M., and Berthoud H.R.: Orexin signaling in the ventral tegmental area is required for high-fat appetite induced by opioid stimulation of the nucleus accumbens. J Neurosci 2007; 27: pp. 11075-11082
- 186. Zheng H., Townsend R.L., Shin A.C., et al: High-fat intake induced by mu-opioid activation of the nucleus accumbens is inhibited by Y1R-blockade and MC3/4R- stimulation. Brain Res 2010; 1350: pp. 131-138
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







