Fig. 5.1
Infraumbilical midline surgery
Massive tear of the peritoneum during TEP: A change to TAPP is highly recommended.
Chronic inguinodynia: In those patients suffering from chronic inguinal pain, once osteomuscular and neuropathic etiologies have been discarded by imaging and physiological testing, a TAPP procedure should be performed if suspicion of an inguinal hernia exists.
Hernia–related factors
Inguinoscrotal hernia: In patients with large inguinoscrotal hernias, the TAPP approach facilitates the reduction of hernia content and aids treatment of the hernia sac mesh placement.
Obesity: Fatty tissue in the abdominal wall in obese patients negatively interferes with the placement and maintenance of the pneumoperitoneum in the preperitoneal space due to the increased weight of the abdominal wall. Due to this, the TAPP approach is the most recommended for obese patients.
Contraindications
Absolute Contraindications
During the last few years, some absolute contraindications have switched to relative contraindications or have even switched to indications. This is due to surgeons’ increased laparoscopic experience [4, 5]:
The laparoscopic repair approach (TAPP) for an inguinal hernia requires a general anesthetic; therefore, patients with an anesthetic risk IV according to the ASA classification are not suitable, and these patients are candidates for a conventional open repair.
Coagulation defects.
Relative Contraindications
Strangulated hernia: The suspicion of hernia strangulated with constricting blood vessels and a difficult reduction of an incarcerated hernia are relative contraindications, as satisfactory results have been reported in such kinds of hernias.
Young patients: Laparoscopic repair with a systematic use of mesh and general anesthesia in young patients is still under debate. For that reason, TAPP is not recommended in patients under the age of 18.
Surgical Technique
Position of the Patient
The patient is positioned in the supine position with both arms next to the body. A table is positioned in the reverse Trendelenburg position in order to push back the small bowel out of the surgical field. A bladder catheter is inserted, and the surgeon stands on the contralateral side to the hernia being treated.
Trocar Position
Once the pneumoperitoneum is established, a 10 mm trocar is placed slightly above the umbilicus. Both 5 mm trocars are placed on both sides of the umbilicus at the medioclavicular lines (Fig. 5.2). In unilateral hernias, an ipsilateral trocar is moved cranially and the contralateral caudally in order to facilitate surgical maneuvers.
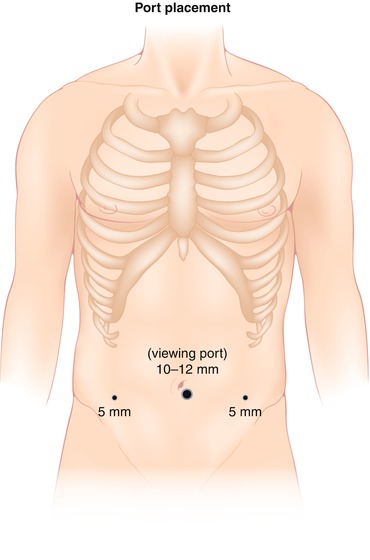
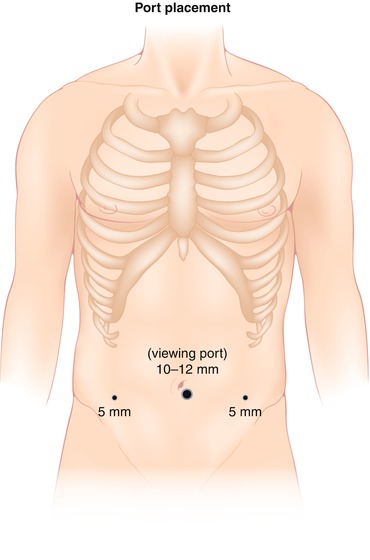
Fig. 5.2
Port placement
Recommended Instruments
A 30° endoscope (10 mm or 5 mm)
One 10 mm trocar and two 5 mm trocars
Two endo-graspers, one endo-dissector, and one pair of endo-shears
Polypropylene mesh (minimum size of 10 × 15 cm, preformatted or not)
Mesh fixation: traumatic (tackers) or atraumatic (biological glues)
Operative Technique
After the creation of the pneumoperitoneum and the trocars are in place, a 30° scope is passed through the 10 mm trocar, the endo-grasper is placed through the 5 mm left-hand trocar, and the endo-shears are placed through the right-hand trocar. The peritoneal cavity of the abdomen is explored. Indirect hernias will be observed laterally to the epigastric vessels and indirect hernias medially to them. The hernia content is gently reduced, and the hernia repair begins by following the next steps:
1.
Peritoneal incision: A horizontal incision of the peritoneum is carried out, 5 cm above the inner inguinal ring, from the anterior superior iliac spine and leading to the paraumbilical ligament. See Fig. 5.3.
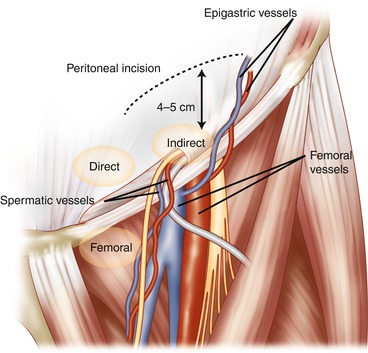
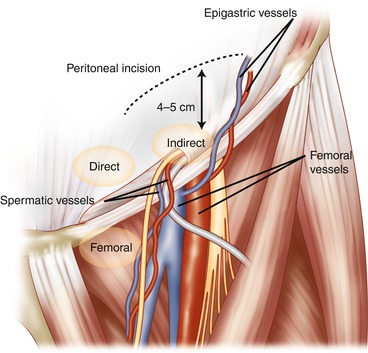
Fig. 5.3
Peritoneal incision
2.
Creation of the preperitoneal space: Dissection of the preperitoneal space, Retzius and Bogros spaces, with identification of anatomical landmarks: epigastric vessels, symphysis, Cooper’s ligament, and iliopubic tract. Laterally, psoas muscle and the femoral cutaneous nerve are observed.
3.
Hernia sac reduction: In cases of direct hernias, the hernia sac is easily reduced with gentle traction caudally; the hernia defect is noted medially above Cooper’s ligament. In cases of indirect hernias, the sac is a continuation of the spermatic cord. The separation of these structures (spermatic vessels and vas deferens) from the sac is mandatory. The vas deferens, a pearly white color, and the gonadal vessels are easily identified in order to try to completely reduce this using traction and contra-traction maneuvers. In cases of large indirect hernias, the sac can be divided with an ENDOLOOP suture. Once the sac is reduced, the preperitoneal space is completely dissected out by performing a parietalization of the cord with the aim of facilitating the proper placement of the mesh.
4.
Mesh introduction and extension: Many meshes have been designed to be used for laparoscopic inguinal hernia repair. Polypropylene is the main polymer used in the manufacture of meshes. Flat or preformed (anatomical) meshes can be used. As to the size of the prosthesis, a minimum size of 10 × 5 cm is recommended (Grade D) in order to diminish recurrence rates. The mesh is introduced through a 10 mm trocar and completely extended in the preperitoneal space, widely covering Cooper’s ligament and three potential hernia sites: the direct, indirect, and femoral rings. See Fig. 5.4.
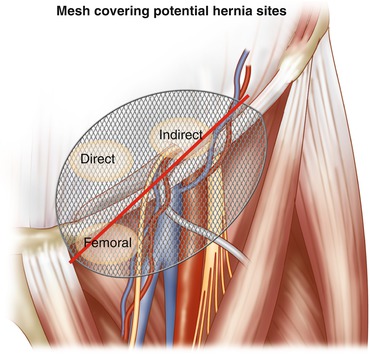
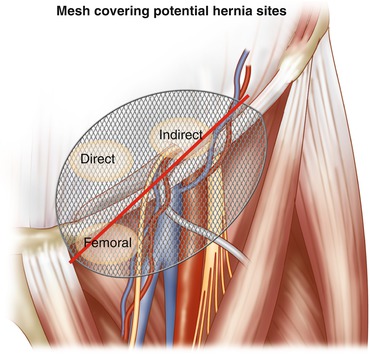
Fig. 5.4
Extended mesh covering potential hernia sites
5.
Mesh fixation: The number of fixation points using helicoidal sutures has decreased over the last few years, from multiple points to just 1 or 2 tackers to Cooper’s ligament, thereby avoiding postoperative pain without increasing recurrence rates. Equivalent results have been published for using non-traumatic fixation of the mesh with fibrin glue. In addition, there are new auto-adhesive meshes which have been developed where no fixation is needed since it is included in the mesh itself [6–8].
6.
The peritoneum is closed over the mesh using a running suture or helicoidal tackers. Nowadays, new self-gripping sutures are used for the peritoneal closure. This kind of new suture facilitates the completion of the TAPP intervention.
7.
Abdominal wall closure: Fascial closure of 10 mm trocar.
Potential Complications and Their Prevention
Intraoperative Complications
This includes all complications related to general anesthesia and the establishment of the pneumoperitoneum. As far as surgical complications are concerned, bleeding is not common and is mainly related to epigastric or gonadal vessel injuries. Electrocautery and/or clips are used to control this bleeding. In order to avoid this, it is necessary to implement gentle handling during traction and contra-traction and to correctly identify all the different structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








