Finding
Cavernous hemangioma
Infantile hemangioma
Anastomosing hemangioma
Capillary hemangioma
Predominant vessel size
Large
Intermediate to small
Small
Small
Anastomosing channels
−
−/+
+
−
Hobnail endothelial cells
−
−
+
−
Plump endothelial cells
−
−/+
−
+
Cytological atypia
−
−
+
−
Lobular pattern of growth
−
−
−
+
Glut 1 staininga
Anticipated to be negative
Anticipated to be positive
Anticipated to be negative
Anticipated to be negative
2.2 Cavernous Hemangioma
2.2.1 Definition
A cavernous hemangioma is a benign vascular tumor with proliferation of dilated, thin-walled vessels.
2.2.2 Clinical Features
Cavernous hemangiomas are the most common benign tumor of the liver and occur in approximately 5 % of all livers. Cavernous hemangiomas occur at all ages, but are most common in young adult women, between the ages of 30 and 50. The tumors can enlarge during pregnancy, or with use of estrogen, but the question of whether or not estrogen is a causal agent for cavernous hemangiomas is unsettled [1–3]. Cavernous hemangiomas are usually diagnosed by imaging studies and biopsies are rarely performed, unless there are atypical imaging findings.
Most patients are asymptomatic, though tumors greater than 4 cm are more likely to present with pain. One study reported that 50 % of individuals with hemangiomas presented with abdominal pain, but in most cases the pain at presentation was related to other diseases, such as irritable bowel syndrome, and not to the hemangioma [4]. Rare cases can also present with a consumptive coagulopathy, called Kasabach-Merritt syndrome [5]. A case has also been reported with high serum AFP levels, which returned to normal after resection of a cavernous hemangioma [6]. The cells producing the AFP were presumably reactive hepatocytes near the edge of the tumor.
2.2.3 Gross Findings
Most (approximately 90 %) of cavernous hemangiomas are single tumors, but in some cases there can be numerous tumors (diffuse hemangiomatosis) [10]. The tumors are well-circumscribed and typically non-encapsulated, with a red brown color and honeycombed appearance. They often have a sponge-like consistency that makes them distinct from adjacent liver parenchyma (Fig. 2.1). Foci of thrombi, fibrosis, and calcification can be noted, especially in larger tumors. In some cases, the hemangioma extends from the surface as a pedunculated mass [11].


Fig. 2.1
Cavernous hemangioma. A subcapsular, well-circumscribed, dark brown-red colored cavernous hemangioma was incidentally identified on liver explant
Some tumors show extensive fibrosis, in which case the vascular nature of the lesion may be less clear. In these cases, the fibrosis typically is more pronounced in the center of the tumor (Fig. 2.2) and in advanced cases, may involve the entire tumor, leading to a firm gray-white sclerotic tumor, called a sclerosed hemangioma (Fig. 2.3) [12].

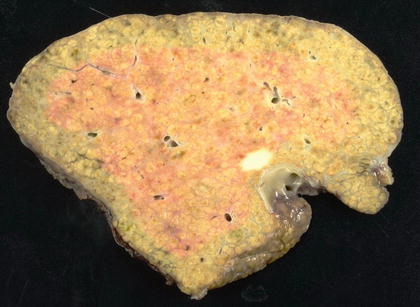

Fig. 2.2
Sclerosing cavernous hemangioma. A large cavernous hemangioma with a central whitish fibrotic area
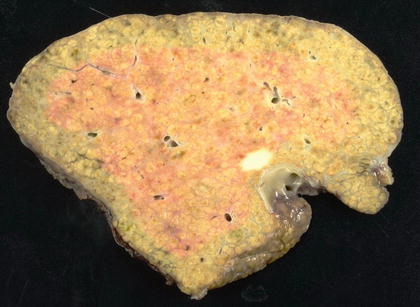
Fig. 2.3
Sclerosed cavernous hemangioma. Only a white, round scar remains
2.2.4 Microscopic Findings
The tumors are composed of a proliferation of large caliber and thin-walled vessels, often filled with red blood cells, within a background of loose fibrous stroma (Fig. 2.4). The vessels are typically lined by flat endothelial cells without atypia or mitoses. Fibrin thrombi and infarction with hemorrhage and hemosiderin-laden histiocytes can also be seen within the tumor (Fig. 2.5). Cavernous hemangiomas have no malignant potential and many will regress with fibrosis over time. In some partially regressed tumors, the vascular proliferation is less apparent and large portions are replaced by myxoid or fibrous tissue, sometimes with focal calcification. In many of these cases, the fibrotic areas coalescence into a central scar (Fig. 2.6). These tumors are often referred to as sclerosing hemangiomas. In one study, there was a modest enrichment for male gender in cases of sclerosing hemangioma [12]. The fibrosis can involve the entire lesion, in which case the term sclerosed hemangioma can be used (Fig. 2.7). Sclerosed hemangiomas typically retain, at least focally, residual hemangioma vessels that allow identification of the tumor [13, 14].
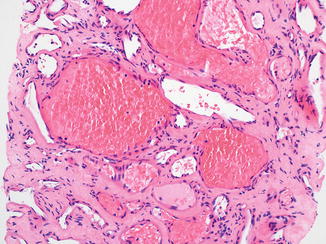
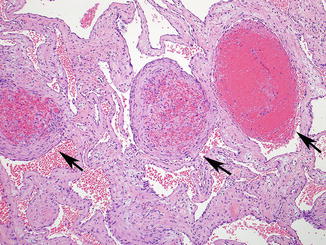
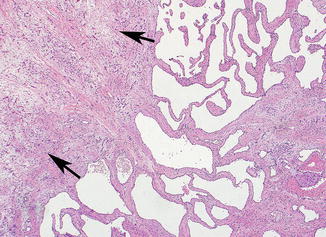
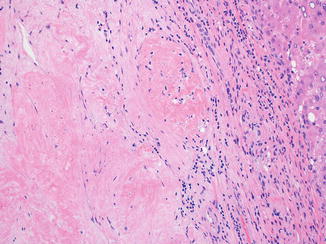
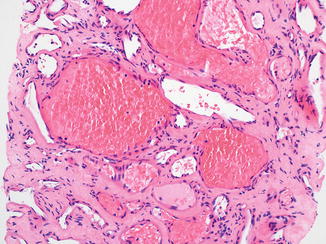
Fig. 2.4
Cavernous hemangioma. Cavernous hemangioma composed of a proliferation of thin-walled and large caliber vessels filled with red blood cells
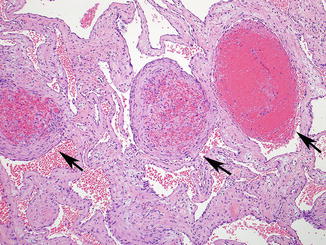
Fig. 2.5
Cavernous hemangioma. The vascular spaces are lined by a single layer of flat endothelial cells without cytological atypia. Fibrin thrombi (arrows) can occur within the vascular channels
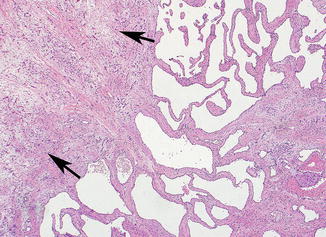
Fig. 2.6
Sclerosing cavernous hemangioma. The hemangioma is partially replaced by myxoid and fibrotic stroma (arrows)
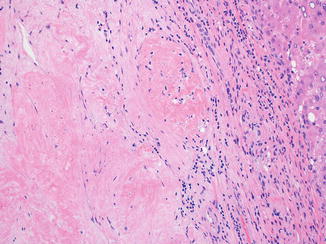
Fig. 2.7
Sclerosed hemangioma. The entire lesion is sclerotic, but vague outlines of vascular channels are apparent
Giant cavernous hemangiomas are defined somewhat variably, but common definitions include size greater than 4 cm or 5 cm [4, 15–17]. Overall, giant cavernous hemangiomas have similar histologic features to smaller cavernous hemangiomas. In approximately 40 % of cases, giant cavernous hemangiomas can have ill-defined borders, with a vascular proliferation that is composed of small aggregates of dilated, telangiectatic, and somewhat smaller-sized vessels as compared to the main tumor. This finding has been called “hemangiomatosis” (Fig. 2.8) [18, 19]. This finding is not unique to large hemangiomas and can also be focally seen at the edges of small cavernous hemangiomas.
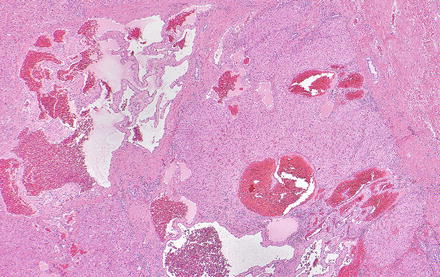
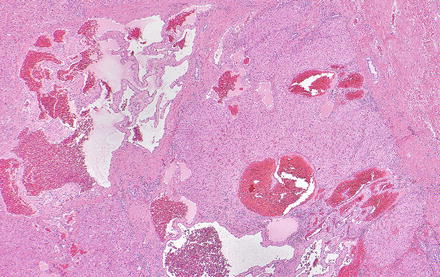
Fig. 2.8
Hemangiomatosis. A small ill-defined vascular proliferation with telangiectatic vessels is present in the liver parenchyma adjacent to a giant cavernous hemangioma
2.2.5 Immunohistochemical Features
A variety of immunohistochemical markers can be used to confirm the presence of endothelial cell proliferation, including CD34, CD31, FLI-1, and ERG.
2.2.6 Differential Diagnosis
Lymphangioma, peliosis hepatis, and hereditary hemorrhagic telangiectasia can mimic cavernous hemangioma. In lymphangioma, the vascular proliferation contains lymph, versus red blood cells in cavernous hemangioma. In addition, lymphangiomas are positive for D2-40 by immunohistochemistry. Peliosis hepatis is characterized by cystic blood-filled spaces without endothelial lining. Hereditary hemorrhagic telangiectasia has distinct histologic features, with inter-anastomosing portal-based vessels and is discussed in more detail in a separate section below.
2.3 Capillary Hemangioma
2.3.1 Definition
A rare variant of benign hemangioma composed of capillary-sized vessels [20]. There has been some debate whether hepatic capillary hemangiomas exit as unique entities, as the “hemangiomatosis” areas at the edges of some cavernous hemangiomas can also have small caliber vessels. However, there are fully resected lesions that appear to be best classified as capillary hemangiomas.
2.3.2 Clinical Features
2.3.3 Gross Findings
Capillary hemangiomas can occur as single or multiple tumors. The tumors are well-circumscribed and can be surrounded by a fibrous capsule.
2.3.4 Microscopic Findings
The tumors are composed of small caliber capillary-sized vessels and the vascular channels are lined by plump endothelial cells without atypia or mitotic activity (Fig. 2.9). The plump cells can sometimes obscure the vascular lumens, and immunostains can be helpful to confirm the vascular nature of the tumor. Foci of extra-medullary hematopoiesis can also be present.
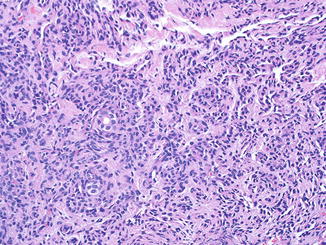
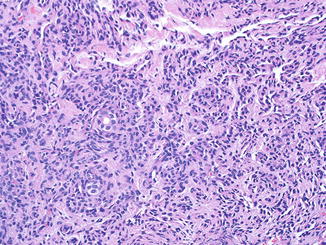
Fig. 2.9
Capillary hemangioma. The tumor is composed of capillary-sized vessels lined by plump endothelial cells. No endothelial cell atypia is present
2.4 Anastomosing Hemangioma
2.4.1 Definition
Benign hemangioma composed of a proliferation of anastomosing, capillary-sized vessels.
2.4.2 Clinical Features
Anastomosing hemangioma is a newly described variant of hemangioma and occurs primarily in the genitourinary tract and adrenal glands [23], but can also be found in the liver. Hepatic anastomosing hemangiomas have been reported to-date in adults, more commonly in women than men [24]. Most cases are incidental findings identified during workup for other processes such as malignancy, back pain, or during abdominal surgery for other causes.
2.4.3 Gross Findings
Hepatic anastomosing hemangiomas present as single tumor ranging from 2 to 6 cm in size. The tumors are grossly well-demarcated with a gray-brown color and spongy appearance.
2.4.4 Microscopic Findings
The tumor is composed of anastomosing capillary-sized vessels with mild cytological atypia and hobnail-appearing endothelial cells, with scant supporting stroma (Figs. 2.10 and 2.11). No mitotic activity is present. Vascular thrombi, extra-medullary hematopoiesis, and hyaline globules can be present. In a subset of cases, a component of more typical cavernous hemangioma can also be present.
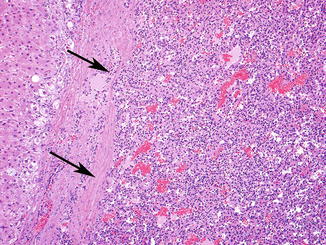
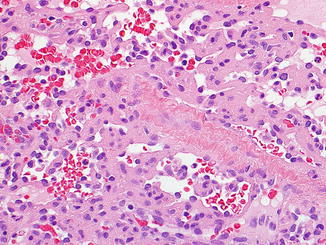
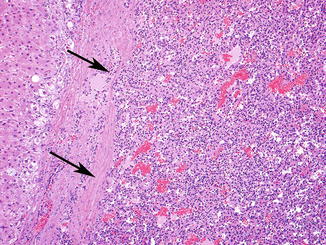
Fig. 2.10
Anastomosing hemangioma. A vascular tumor (arrows) with proliferation of anastomosing capillary-sized vessels
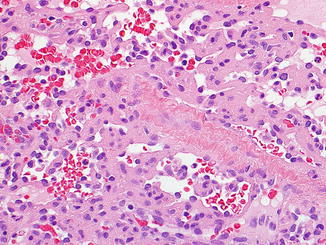
Fig. 2.11
Anastomosing hemangioma. The endothelial cells have a hobnail appearance and mild cytological atypia, but no mitotic activity
2.4.5 Immunohistochemical Findings
The panel of immunohistochemical stains (CD34, CD31, FLI-1, and ERG) used for diagnosing cavernous hemangiomas can also be used for anastomosing hemangiomas (Fig. 2.12).
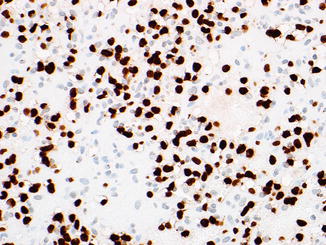
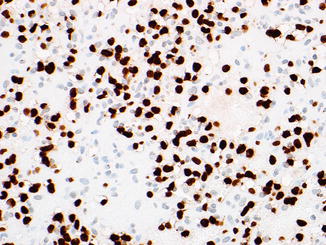
Fig. 2.12
ERG immunostain. This anastomosing hemangioma is strongly ERG-positive
2.4.6 Differential Diagnosis
The main differential diagnosis for anastomosing hemangiomas is angiosarcoma, due to the anastomosing growth pattern and the mild cytological atypia. However, the lack of marked atypia, the low proliferative rate, and the distinctive hob nail cells can assist in identifying this rare variant of hepatic hemangioma and avoid a misdiagnosis of angiosarcoma.
2.5 Infantile Hemangioma in Adults
Infantile hemangiomas are discussed in more detail in Chap. 13. The vast majority of cases occur in infants and young children, but rare cases have been reported in adults [25]. They should be diagnosed in the same way as in infants and children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








