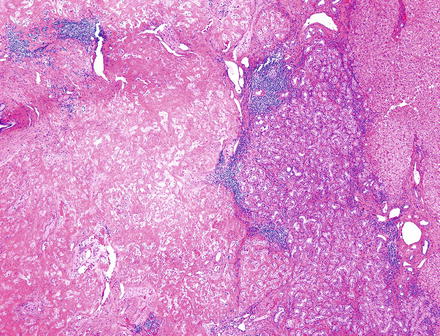
Fig. 5.1
Ciliated hepatic foregut cyst. The wall of ciliated hepatic foregut cyst has four layers: ciliated epithelium, subepithelial connective tissue, smooth muscle, and fibrous stroma
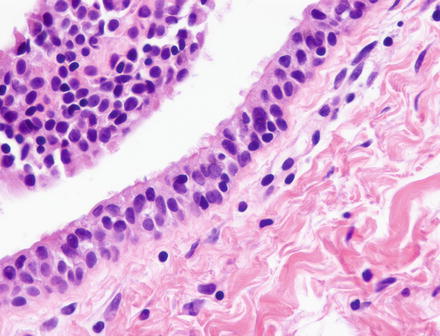
Fig. 5.2
Ciliated hepatic foregut cyst. Cilia are visible on the surface epithelial cells
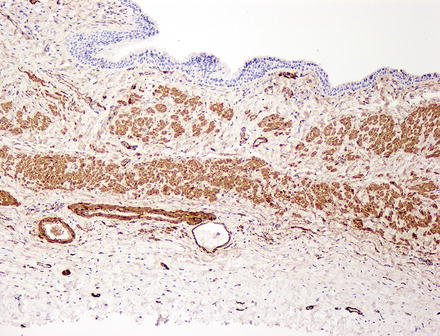
Fig. 5.3
Ciliated hepatic foregut cyst. Immunostain for smooth muscle actin shows bundles of smooth muscle without an organized structure
There are at least five reports of squamous cell carcinoma arising in ciliated hepatic foregut cyst [9–13]. As might be expected, cysts complicated by malignancy tend to be large and have solid or firm areas in the cyst wall. Four of the five reports noted squamous metaplasia in the cyst lining. Two patients developed intraabdominal recurrence within 1 year of surgery, one of whom died.
5.1.5 Differential Diagnosis
The clinical differential diagnosis includes solitary bile duct cyst, Echinococcal cyst [14], and solid tumors with cystification. Histologically, the diagnosis should be straightforward, given the characteristic ciliated lining and the smooth muscle in the wall. While previously regarded as universally benign, recent reports of malignancy suggest that careful sampling to rule out carcinoma is appropriate, particularly in cysts with squamous metaplasia.
5.2 Biliary Adenofibroma
5.2.1 Definition
Biliary adenofibroma is a rare benign biliary tumor of unknown etiology, first described in 1993 [15]. It features dilated tubules lined by cuboidal epithelium, set in a dense fibrous stroma. In this sense, it resembles an enlarged version of a von Meyenburg complex, an entity with which it shares immunohistochemical characteristics.
5.2.2 Clinical Features
There are fewer than ten cases reported in the literature, all in adults, with roughly equal sex distribution. The clinical presentation generally features right upper quadrant pain, although a few cases have been discovered incidentally at surgery. Initial reports suggested indolent behavior, although Varnholt et al., reporting the third known case noted strong nuclear staining for p53 in 50–75 % of tumor nuclei [16].
5.2.3 Gross Findings
Biliary adenofibromas form firm, circumscribed mass, usually white or tan, that range in size from 5 to 20 cm. They are not so much cystic as “microcystic” or “honeycombed.” Individual cysts range in size from 0.1 to 0.5 cm and contain nonmucinous fluid.
5.2.4 Microscopic Findings
Low power examination shows a complex network of tubulopapillary cysts embedded in fibrous stroma (Fig. 5.4). The cysts are lined by cuboidal or low columnar epithelium arranged in a single layer (Fig. 5.5). Tumor nuclei are round or oval, with inconspicuous nuclei and, often, apocrine snouts (Fig. 5.6). In one reported case, some tubules contained amorphous material resembling bile. There are very rare reports of malignant transformation [17], and Nguyen et al. described high-grade dysplasia in a biliary adenofibroma [18]. Our own files include a biliary adenofibroma giving rise to cholangiocarcinoma (Figs. 5.7, 5.8 and 5.9).
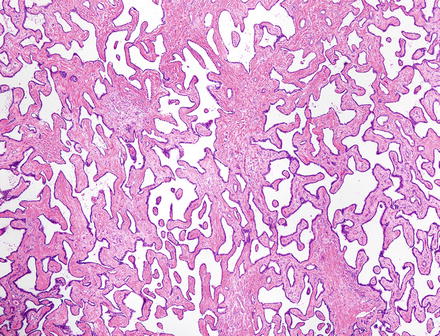
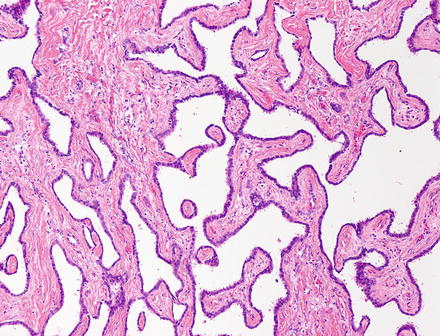


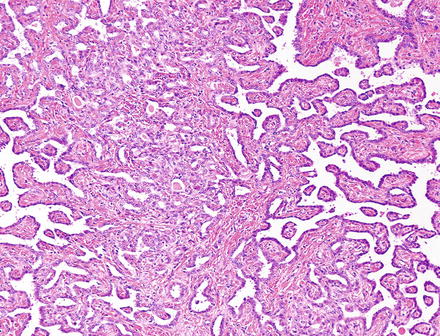
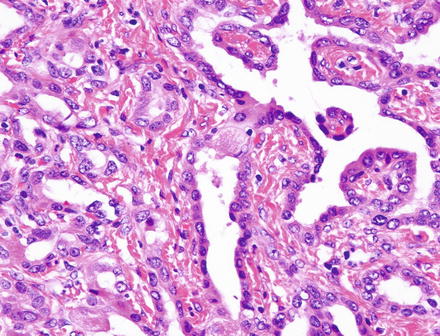
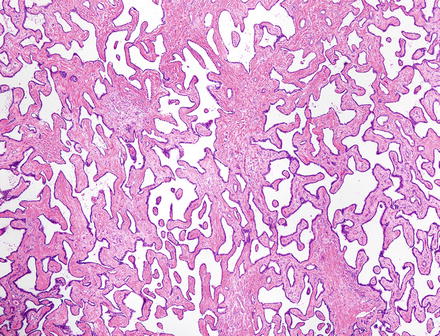
Fig. 5.4
Biliary adenofibroma. Irregularly shaped cystic tubules, some with papillae
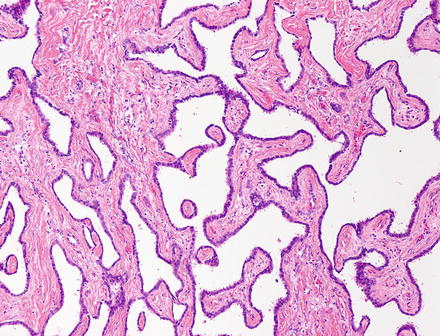
Fig. 5.5
Biliary adenofibroma. The spaces of biliary adenofibroma are lined by a single layer of cuboidal epithelium. The stroma is bland and sparsely cellular

Fig. 5.6
Biliary adenofibroma. The cells of biliary adenofibroma have oval and regular nuclei. Many cells have apocrine snouts

Fig. 5.7
Cholangiocarcinoma arising in biliary adenofibroma, gross. The benign component is the white area in the lower right
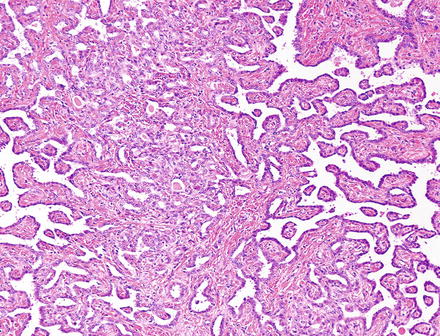
Fig. 5.8
Cholangiocarcinoma arising in biliary adenofibroma. Adenofibroma is at the left and right edges, with cholangiocarcinoma in the center
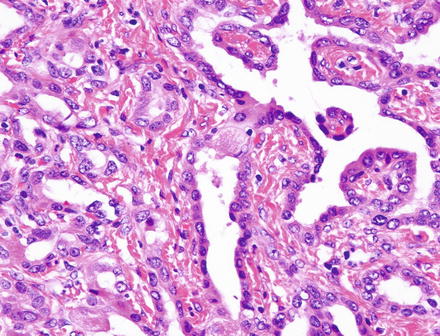
Fig. 5.9
Cholangiocarcinoma arising in biliary adenofibroma. Transition from adenofibroma (right) to carcinoma (left). The nuclei in the adenofibroma component are larger, darker, and more irregular than those seen in Fig. 5.6
5.2.5 Immunohistochemical Features
The lining cells express pankeratins, cytokeratin 7, cytokeratin 19, carcinoembryonic antigen, and epithelial membrane antigen. They are also positive for D10 and negative for 1F6, a pattern also seen in von Meyenburg complexes, which suggests derivation from bile ducts rather than ductules or peribiliary glands [19].
5.2.6 Differential Diagnosis
The differential diagnosis includes bile duct adenoma and mucinous cystic neoplasm. The tubules of bile duct adenomas are less dilated and more closely packed. Some examples of bile duct adenoma are dominated by stroma, but in these cases the tubules are compressed by the stroma rather than dilated. Bile duct adenomas often produce mucin; biliary adenofibromas do not, and in fact may contain bile. Mucinous cystic neoplasm also produces mucin, but the main differentiating feature here will be the cellular mesenchymal (ovarian-like) stroma that should be present at least focally in virtually all mucinous cystic neoplasms.
5.3 Solitary Bile Duct Cyst
5.3.1 Definition
The solitary bile duct cyst (also known as simple cyst) is a unilocular cyst lined by a single layer of cuboidal epithelium atop a layer of fibrous tissue. It can occur at any age, but generally presents in middle adulthood. There is a substantial but unexplained female preponderance.
5.3.2 Clinical Features
Solitary bile duct cysts arise in the right lobe more often than the left. They have a strong female predominance (8:1) and are usually seen in the sixth decade of life. There are a handful of case reports describing carcinoma arising in solitary bile duct cysts, the most recent example being a 1988 description of squamous cell carcinoma arising in a background of squamous metaplasia [20].
5.3.3 Gross Findings
Solitary bile duct cysts are single, round, and unilocular, usually with a smooth inner lining (Figs. 5.10 and 5.11). Occasionally, there can be an aggregate of multiple smaller cysts. When septa are present, they tend to be thin and situated at the periphery of the cyst, a feature that helps in the CT distinction of solitary bile duct cysts from mucinous cystic neoplasms and intraductal papillary biliary neoplasms [21]. The cyst contents are clear, unless they have been altered by infection or hemorrhage. Some bile duct cysts connect to the biliary system and may contain bilious fluid.
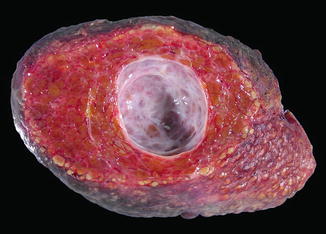
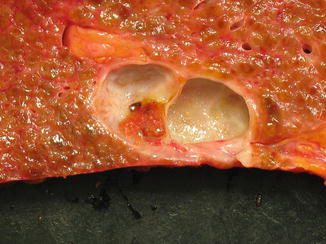
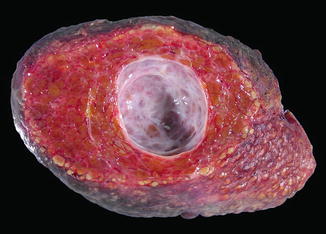
Fig. 5.10
Solitary bile duct cyst, gross. The lesion forms a unilocular cyst. The lining is smooth except for a few slender septa at the periphery
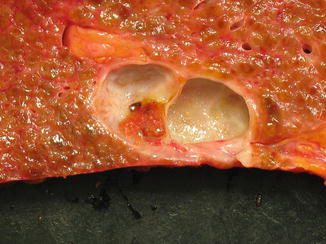
Fig. 5.11
Solitary bile duct cyst, gross. Another example showing amorphous material adherent to the wall
5.3.4 Microscopic Findings
The solitary bile duct cyst is lined by a single layer of cuboidal epithelium resting on a layer of connective tissue (Fig. 5.12). The epithelium is often disrupted (Fig. 5.13) and may be completely denuded. When the epithelium is lost, it can be replaced by a layer of blood and fibrin (Fig. 5.14). The lining epithelium may sometimes undergo intestinal, pyloric, or squamous metaplasia (Fig. 5.15). No ovarian type stroma should be seen underneath the epithelium.
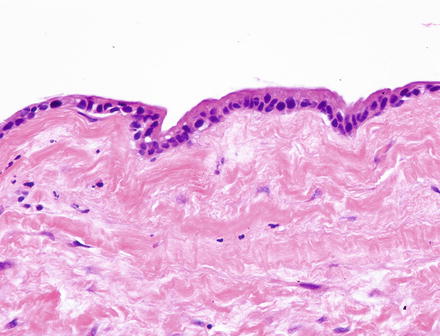
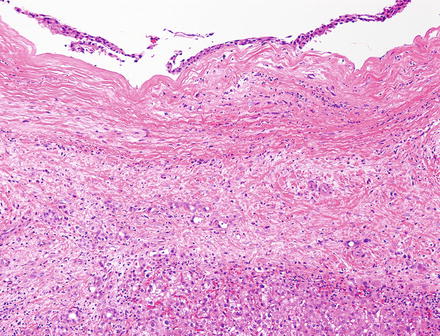
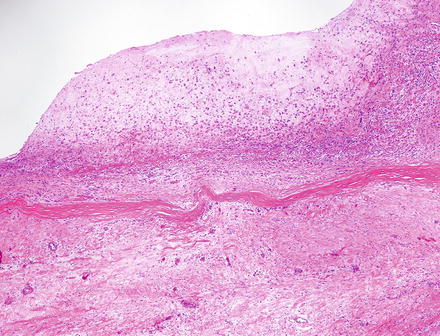
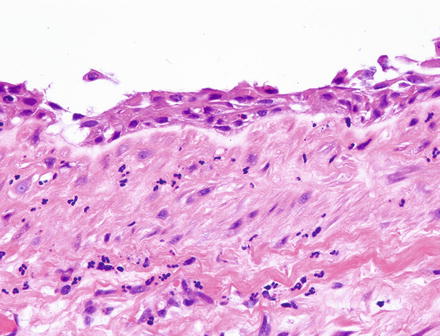
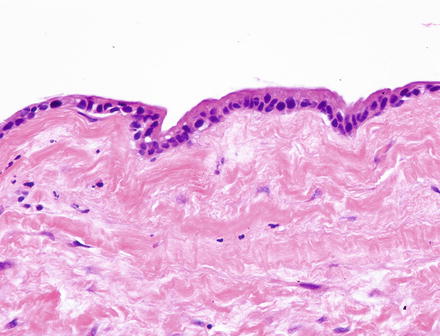
Fig. 5.12
Solitary bile duct cyst. Bland cuboidal epithelium atop a layer of fibrosis
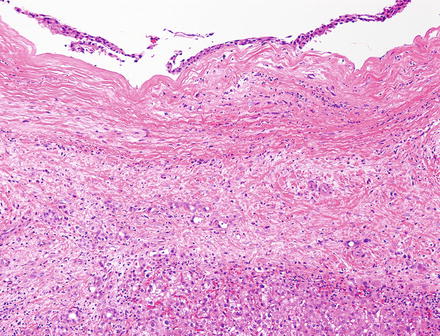
Fig. 5.13
Solitary bile duct cyst. Partial stripping of the cuboidal epithelium. The absence of fibrin or blood suggests that this occurred during tissue processing
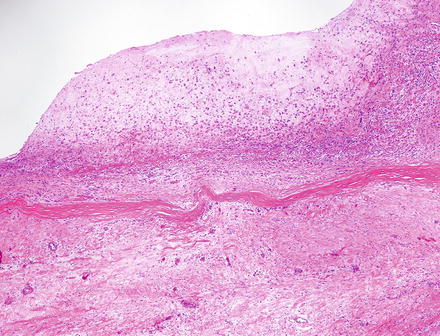
Fig. 5.14
Solitary bile duct cyst. The epithelium is replaced by fibrin, blood, and inflammation in the denuded area
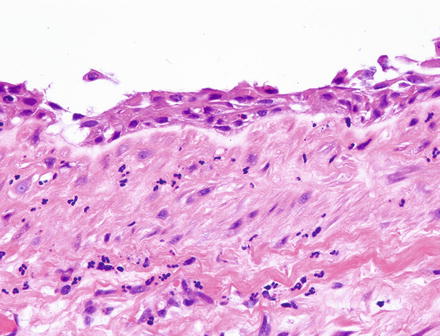
Fig. 5.15
Solitary bile duct cyst. Squamous metaplasia of the lining epithelium
5.3.5 Differential Diagnosis
The primary entity in the differential diagnosis is the mucinous cystic neoplasm. While the lining in mucinous cystic neoplasms is characteristically mucinous, it too can be damaged and denuded. Extensive sampling to document either cuboidal or mucinous epithelium may be necessary. The ovarian-like stroma of mucinous cystic neoplasm is not present in every section, and its demonstration also may require extensive sampling. In difficult cases, histochemical stains for mucin and immunohistochemical stains for estrogen receptor and progesterone receptor are helpful. Mesothelial cysts have a lining morphologically similar to bile duct cyst, but the former are small, subcapsular, and rare; immunohistochemistry for markers of mesothelial lineage such as calretinin are helpful if the question of mesothelial cyst arises. Ciliated hepatic foregut cyst and enteric duplication cysts have a different lining and smooth muscle in the cyst wall. Extensive denudation in a solitary bile duct cyst can lead one to also consider Echinococcal cyst, prompting a search for the inner laminated membrane, protoscolices and hooklets characteristic of that process.
There are no histologic features that allow one to differentiate between solitary bile duct cyst and the cysts of polycystic liver disease or liver involvement by polycystic kidney disease. Clinical history and imaging studies are informative in this setting. The multiple hepatic cysts of autosomal dominant polycystic disease are always accompanied by multiple von Meyenburg complexes, providing an additional clue to the diagnosis.
5.4 Bile Duct Adenoma
5.4.1 Definition
The bile duct adenoma is a benign proliferation of compact ductal structures lined by cuboidal epithelial cells. The classic review of 152 bile duct adenomas from the AFIP proposed that this is a reactive ductular proliferation [22], but there is also evidence for origin from peribiliary glands rather than bile ducts or ductules, thus the alternative name of peribiliary gland hamartoma [19].
5.4.2 Clinical Features
These lesions are asymptomatic, and are almost always incidental findings at surgery, biopsied to rule out malignancy. They are rare in autopsy series as suggested by Cho et al., who found only 13 cases of bile duct adenomas in 2,125 cases [23] but seem to be increased in the setting of chronic liver disease. Aishima et al., for example, reviewed a mix of resected hepatocellular carcinomas (n = 1,306) and livers explanted for cirrhosis (n = 150) and found 35 cases with bile duct adenomas (2.4 %) [24].
5.4.3 Gross Findings
Bile duct adenomas form small tumors (usually <1 cm) that are white, well circumscribed, and generally situated immediately beneath the liver capsule. In the AFIP series, 83 % of bile duct adenomas were solitary [22].
5.4.4 Microscopic Findings
Histologic examination shows a round or oval, well demarcated but not encapsulated nodule, often with increased lymphocytes and lymphoid aggregates at the periphery (Figs. 5.16 and 5.17). Preserved portal tracts are present inside the nodule or immediately adjacent to it. The nodule is populated by small, uniform tubules lined by cuboidal epithelium with round, regular nuclei (Fig. 5.18). Nucleoli are not prominent and mitotic activity is absent. The cells can produce mucin but not bile. The tubules are generally round to oval but may take on more serpentine, complex pattern (Figs. 5.19 and 5.20). When there is substantial fibrous stroma, the tubules may be compressed into curved slits (Fig. 5.21). Bile duct adenomas differ histologically from reactive bile ductular proliferations, as demonstrated in Fig. 5.22, which shows a bile duct adenoma immediately adjacent to a focus of reactive ductular proliferation.
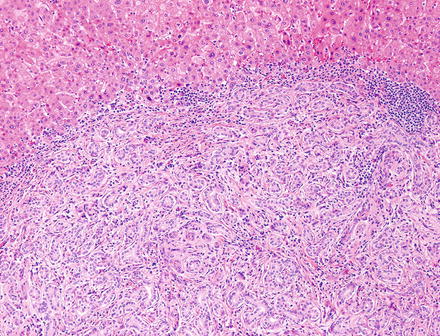
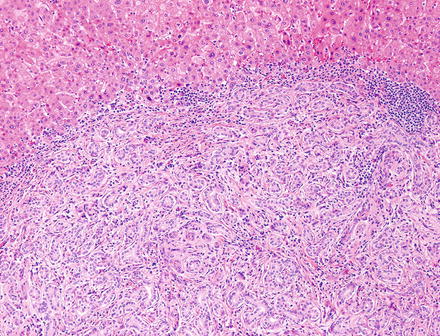
Fig. 5.16
Bile duct adenoma. Slender cuff of lymphocytes at the periphery