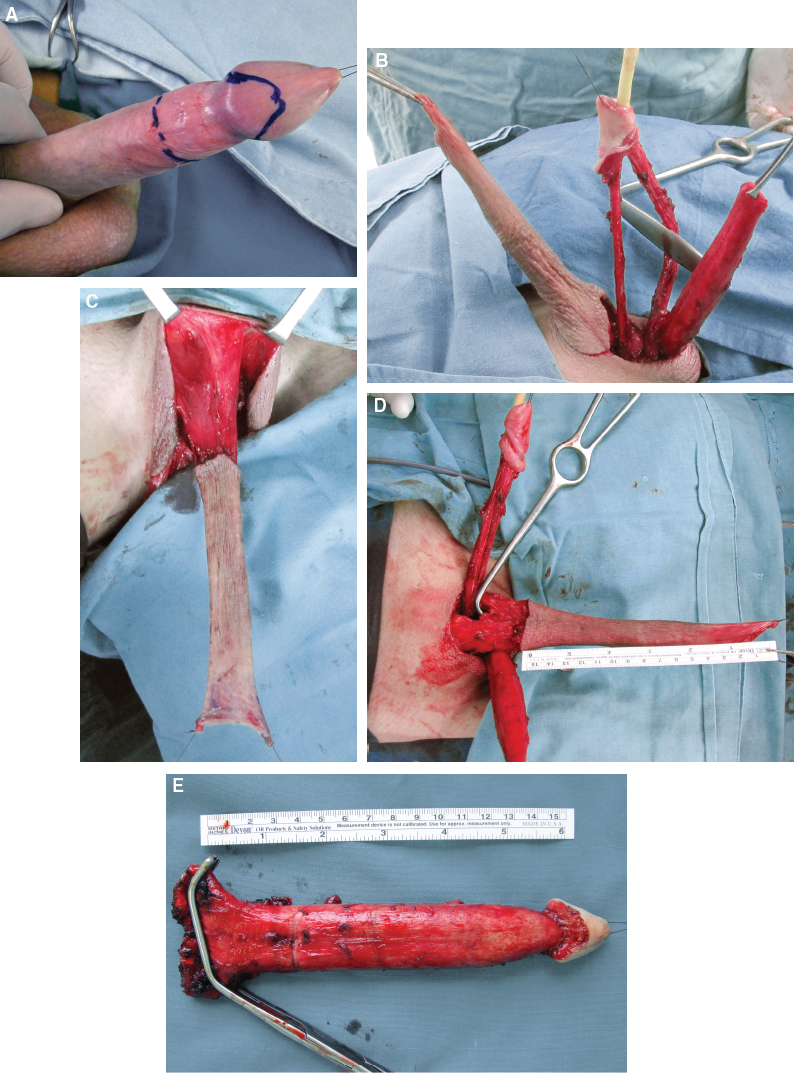
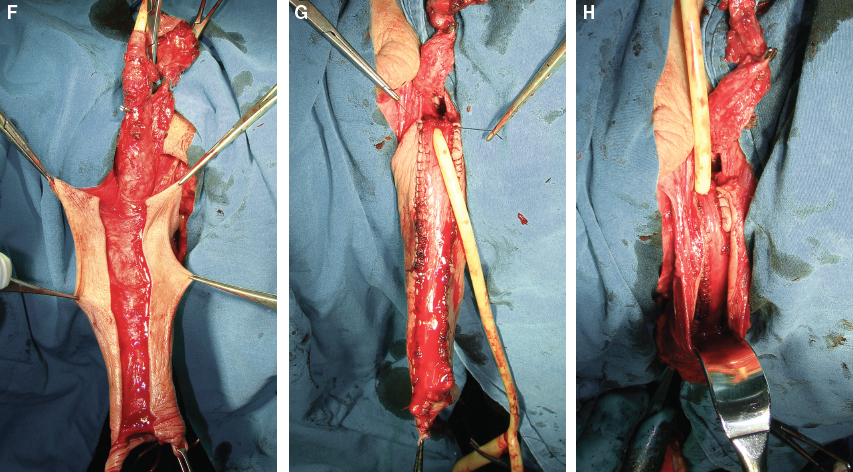
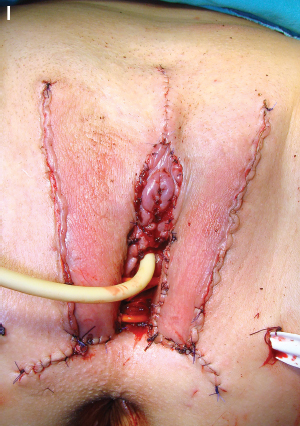
CHAPTER 5 Vaginal absence has a devastating impact on a biologic woman or male-to-female transgender patients. Thus, in such patients, it is essential to create a normal functioning neovagina with satisfactory sexual function and aesthetic appearance. Vaginal reconstruction is inevitable in the case of vaginal agenesis, disorders of sexual development, transsexualism, defects resulting from genital cancer surgeries, and trauma. There are many reports on various surgical procedures, their outcomes after postoperative complications, and anatomic and functional results.1–6 Some popular methods include split-thickness and full-thickness skin grafts, bladder or buccal mucosa grafts, penile or penoscrotal skin flaps, local genital flaps, and intestinal flaps.1–6 Skin grafts are used frequently because of their simplicity and the fact that they are associated with fewer complications. In transsexual patients with a preserved penis and scrotum, use of penile and penoscrotal skin flaps remains the method of choice. However, these methods have certain disadvantages, such as scarring, shrinkage, an insufficient vaginal cavity, intravaginal hair growth, the need for lubrication during intercourse, and permanent dilation. The debate on surgical management of this condition with the very large number of techniques that have been described continues, and considerable controversy still exists over which is the best technique to choose. Surgical techniques should be classified by the type of flap or graft that will be used for vaginal reconstruction. The types of flaps or grafts include penile/penoscrotal skin grafts, pedicled penile/penoscrotal flaps, free skin grafts, bladder mucosa, include intestinal segments.7,8 The aesthetic, sensational, and functional results of vaginoplasty vary greatly. Surgeons vary considerably in their techniques and skills, patients’ skin varies in elasticity and healing ability, previous surgery in the area can have an impact on results, and surgery can be complicated by problems such as infections, blood loss, or nerve damage. However, in the best cases, when recovery from surgery is complete, it is often very difficult for anyone, including gynecologists, to detect women who have undergone vaginoplasty. Supporters of colovaginoplasty argue that this method is better than the use of skin grafts, because the colon is already mucosal, whereas skin is not. However, many transwomen report postoperatively that the skin used to line their vaginas develops mucosal qualities within months to years after surgery. For others, lubrication during intercourse is necessary, and occasional douching is advised to prevent the growth of bacteria and the resulting odors. Because the human body treats the new vagina as a wound, any current technique of vaginoplasty requires some long-term maintenance of volume (vaginal dilation) by the patient with medical graduated dilators, dildos, or suitable substitutes to keep the vagina open. Sexual intercourse is not always an adequate method of performing dilation. In our center for transgender surgery, the inverted penile skin-flap technique still remains the first choice for vaginoplasty in transsexual patients.9 In this chapter, we describe our technique of skin-flap vaginoplasty in male-to-female transsexual patients. There are several advantages to penile skin-flap vaginoplasty. As a flap, penile skin has less tendency to contract, better local innervation and sensibility of the neovagina, and yields a hairless and natural-colored neovagina.2,8–10 Many patients are able to have a normal sex life postoperatively, although the level of satisfaction in this population varies. Psychosocial and psychosexual outcomes lead us to understand the significance of surgical repair and the impact on the patient’s and partner’s life after surgery. Also, because postoperative complications and pitfalls give rise to numerous physical and psychological problems, it is important that they be recognized and corrected in a timely manner. Before sex reassignment surgery, all patients must have complete Standards of Care for Gender Identity Disorders (SOC) documentation. The most widespread SOC in this field is published by the World Professional Association for Transgender Health, previously known as the Harry Benjamin International Gender Dysphoria Association.14 A preoperative assessment of all patients includes clinical examination of the external genitalia, echosonography of the testicles, cystoscopy, and a full hormonal profile. Patients are admitted to the hospital the day before surgery for mechanical bowel preparation with an enema; 2 g of ceftriaxone and 500 mg of metronidazole are administered intravenously with the induction of anesthesia. Preoperative planning includes estimation of the proper size and position of the neoclitoris based on the patient’s preferences. In the case of hairy penile skin, preoperative laser epilation is recommended to prevent a hairy neovagina. To form the new vagina, several subprocedures must be performed: orchiectomy, removal of the corpora cavernosa, creation of the neovaginal cavity, vaginoplasty, lining of the cavity with the urethral orifice and vaginal introitus, clitoroplasty, and labioplasty. After the usual bilateral orchiectomy, the penis is dissected into its anatomic components; that is, the corpora cavernosa, the glans cap with the urethra and neurovascular bundle, and the vascularized penile skin (Fig. 5-1, A and B). This principle, called the penile disassembly technique, presents the main advantage, because it allows the ideal use of all penile components (except the corpora cavernosa) in the construction of the new vulva, clitoris, and vagina.15,16 The glans, with the neurovascular bundle dorsally and urethra ventrally, is lifted from the tips of the corpora cavernosa together with Buck fascia, thus completely preserving these components (Fig. 5-1, C). As the glans cap is divided into two, the dorsal part of the glans is reduced by excising the central ventral tissue, leaving the sides of the glans intact. This is used to create the neoclitoris. Lateral excisions on the glans are not recommended to avoid injuring the neurovascular bundle, which enters the glans cap lateroventrally. However, the sides are deepithelialized and sutured to achieve a conical shape and appropriate size for the neoclitoris, with preserved vascularization and sensitivity (Fig. 5-1, D). The penile disassembly also provides ideal exposure of the corpora cavernosa for their removal at the level of attachment to the pubic rami. Short remnants of the corpora cavernosa (erectile tissue) are also destroyed to prevent any postoperative erection that could hinder sexual intercourse (Fig. 5-1, E). Fig. 5-1 A, Preoperative appearance of male genitalia. B, All penile structures are disassembled—the glans with the neurovascular bundle dorsally and the urethra ventrally, corporeal bodies, and penile skin. C, Penile skin is dissected with a long vascular pedicle to enable insertion of the neovagina into the perineal space. D, The clitoris is created with the dorsal part of the glans, which is sutured after excising the central ventral tissue. A hole at the base of the skin flap is created. The neoclitoris and male urethra are transposed dorsally. E, Corporeal bodies are completely removed from the bones. F, A superficial incision is made at the dorsal part of penile skin, whereas the vascularized subcutaneous tissue remains intact. G, The urethra is spatulated up to its bulbar part. The urethral flap is embedded into the skin tube and sutured to the skin edges. H, The vagina is fashioned by inversion of the penile skin and urethral flap. I, Appearance at the end of surgery. The vagina is placed into the cavity and fixed to the sacrospinous ligament. Labia minora and labia majora are created from the remaining penile and scrotal skin.
Male-to-Female Gender Affirmation Skin-Flap Vaginoplasty
Key Points
 The penile inversion technique is one of the best solutions to vaginal reconstruction in male-to-female transgender patients.
The penile inversion technique is one of the best solutions to vaginal reconstruction in male-to-female transgender patients.
 The penile disassembly technique enables radical removal of the corpora cavernosa, which prevents postoperative complications such as postoperative erections, painful sexual intercourse, and psychological disturbances.
The penile disassembly technique enables radical removal of the corpora cavernosa, which prevents postoperative complications such as postoperative erections, painful sexual intercourse, and psychological disturbances.
 A vascularized urethral flap is a good option for the mucosal part of the neovagina and should be used to ensure better moisture of the neovagina postoperatively.
A vascularized urethral flap is a good option for the mucosal part of the neovagina and should be used to ensure better moisture of the neovagina postoperatively.
 Fixation of the neovagina to the sacrospinous ligament is the key to successfully preventing postoperative prolapse.
Fixation of the neovagina to the sacrospinous ligament is the key to successfully preventing postoperative prolapse.
 Postoperative dilation of the neovagina is mandatory in first 6 months after surgery.
Postoperative dilation of the neovagina is mandatory in first 6 months after surgery.
Clinical Evaluation
Indications and Contraindications
Preoperative Planning and Preparation
Surgical Techniques
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree