and Hubert Lepidi1
(1)
UER Médecine, Aix-Marseille Université, Marseille, France
Abstract
This innervation is extremely important, not only due to its density but also due to the major role it plays in sexual life. It consists of a double innervation, which is, on the one hand, cerebrospinal and, on the other hand, vegetative. The pudendal nerve (shameful nerve), cerebrospinal contingent, is the key component and has therefore been referred to as “king of the perineum” (R. Robert et al.). However, it is not the only nerve structure to be involved. The other key nerve contingent is the vegetative contingent, originating from the inferior hypogastric plexus: the cavernous nerve of the clitoris. Such as will be noted in the following sections, the two components converge and meet to ensure the extraordinary innervation of the bulbo-clitoral organ.
8.1 General
This innervation is extremely important, not only due to its density but also due to the major role it plays in sexual life. It consists of a double innervation, which is, on the one hand, cerebrospinal and, on the other hand, vegetative.1 The pudendal nerve (shameful nerve), cerebrospinal contingent, is the key component and has therefore been referred to as “king of the perineum” (R. Robert et al.). However, it is not the only nerve structure to be involved. The other key nerve contingent is the vegetative contingent, originating from the inferior hypogastric plexus: the cavernous nerve of the clitoris. Such as will be noted in the following sections, the two components converge and meet to ensure the extraordinary innervation of the bulbo-clitoral organ.
8.1.1 Pudendal Nerve
The anatomy of the pudendal nerve (shameful nerve according to former authors) is better known since a number of specialists, and a team from Nantes2 (already mentioned above) in particular, have focused their attention on the investigation of the causes of positional perineal pains and the discovery of neuralgia by “pudendal nerve entrapment syndrome”.
The pudendal nerve is the terminal branch of the pudendal nerve plexus dedicated to external genitals and the perineum. The pudendal plexus is most generally plexiform and formed by the fusion of the fibres from the ventral branches of spinal nerves S2, S3 and S4. This plexus originates from the true pelvis and ends as a single trunk: the pudendal nerve.
As soon as it has formed, the nerve leaves the true pelvis, crosses the greater ischiatic incisure (greater sciatic foramen) in the infrapiriformis canal (sub-pyramidal canal) and reaches the gluteal region (buttocks region). It rapidly leaves the latter and passes through the true pelvis again by circumventing the ischial spine (sciatic spine) and by crossing the lesser ischiatic incisure (lesser sciatic foramen). It passes through the true pelvis, with the artery and the pudendal veins (shameful internal vessels), against the internal surface of the ischial tuberosity, and follows the lateral wall of the ischio-rectal fossa by engaging through a fibrous tunnel, Alcock’s pudendal canal (shameful canal). This canal consists of the fascia of the obturator internus muscle and arched fibres stretched between this fascia and the falciform process of the sacrotuberous ligament (greater sacro-sciatic ligament). It is in the first centimetres of this fibre canal that the pudendal nerve forms an important collateral branch: the inferior rectal nerve. It then divides into its 2 terminal branches: the perineal nerve and the dorsal nerve of the clitoris.3
The perineal nerve will, in turn, divide at the posterior edge of the anterior perineum (urogenital perineum), into a superficial perineal nerve and a deep perineal nerve:
The superficial perineal nerve is a sensory nerve. It is dedicated to the teguments of the perineum (posterior labial nerves dedicated to the posterior part of the labia majora) and to the external orifice of the urethra.
The deep perineal nerve, once it has circumvented the posterior edge of the deep transverse muscle, is successively routed in the deep space and then in the superficial space of the anterior perineum. Its motor contingent supplies the ischiocavernosus and bulbospongiosus muscles, muscles of the erectile bodies of the bulbo-clitoral organ. Its sensory fibres are dedicated to the major vestibular gland, the spongy bulb and partly to the vestibule.
The dorsal nerve of the clitoris extends in the direction of the pudendal nerve and remains in the pudendal canal, along the ischio-pubic branch, which it will follow to join the clitoris.
Such as we have just observed, all is clear for the anatomy of the pudendal nerve. So much cannot be said for the anatomy of the dorsal nerve of the clitoris. Not many studies have been conducted on this nerve until recently.
Considering the importance of this nerve and the observations that we have been able to make during our dissections, its specific study proves to be essential and will be conducted later.
8.1.2 Cavernous Nerve of the Clitoris
It is this nerve which leads the contingent of fibres of the autonomic nervous system (vegetative nerve fibres) to the erectile bodies. Its fibres originate from the uretro-vaginal part of the inferior hypogastric plexus (Fig. 8.7), plexus pair located in the sub-peritoneal cellular tissue, which coats the lateral surfaces of the female pelvis.
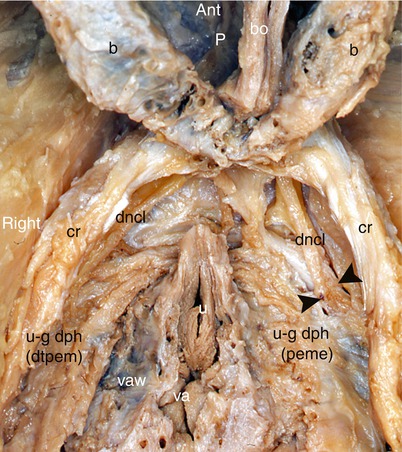
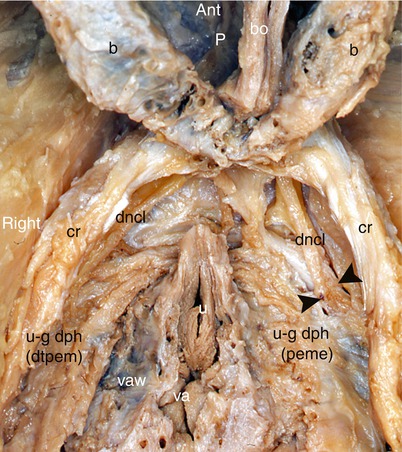
Fig. 8.1
The dorsal nerves of the clitoris in their ischio-pubic initial segment (dissection of the female anterior perineum, gynaecological position). The bulbs and the clitoris were folded against the pubis. The crura were released from their fibrosis attachments and pushed slightly outside. b bulb, bo clitoral body (descending part), cr crus of clitoris, dncl dorsal nerve of clitoris, p pubic symphysis, u external urethral orifice, u–g dph uro-genital diaphragm, dtpem deep transverse perineal muscle (visible on the right, after resection of the perineal membrane), u–g dph (peme) perineal membrane, va vaginal orifice, vaw vaginal wall, black arrowheads they line the banks of the incision of the perineal membrane making the nerve, which still remains in the deep perineal space, visible. Note the oblique course of the dorsal nerve of the clitoris, going forwards and within
Each plexus is formed by the plexiform convergence of ortho- and parasympathetic fibres.4 The following fibres are included in its composition:
Orthosympathetic nerve fibres: They are the sacral splanchnic nerves—they come from the pelvic sympathetic ganglia (sacral sympathetic ganglia).
Parasympathetic nerve fibres, an important contingent from the pelvic splanchnic nerves (Eckard’s erectile nerves), collateral of the pudendal plexus, originating from the ventral roots of sacral nerves S2, S3 and S4.
Mixed nerve rami from the superior hypogastric plexus (inter-iliac plexus or presacral nerve of Latarjet), which conveys both the orthosympathetic and parasympathetic fibres.
The efferent branches of the inferior hypogastric plexus are dedicated to the rectum (medium rectal nerves), the uterus, the vagina, the bladder, the clitoris and the bulbs.
Thus, the vegetative nerve fibres dedicated to the clitoris are routed thereto via the 2 cavernous nerves, which originate from this inferior hypogastric plexus.
8.1.3 Descriptive and Topographic Anatomy of the Clitoral Innervation
8.1.3.1 Dorsal Nerve of the Clitoris
The dorsal nerve of the clitoris has, up until recent times, rarely been studied and therefore is badly known, especially since few authors have had the curiosity to reread the remarkable work conducted by Kobelt and, even more exceptionally, the will to study the said nerve by dissection. However, respecting the integrity of this nerve guarantees that the functionality of the clitoris will not be compromised and, therefore, that an essential and key part of female sexuality will not be affected.
This nerve is at the centre of many surgical acts: treatment of fractures of the pelvis, reduction of symphysis disjunctions, surgery of the urethra, repair surgery of certain lower urogenital congenital anomalies (Baskin L.S.), clitoridoplasties, surgery of tumours of the pubis, installation of trans-obturator tape for treating urinary incontinence (Achtari C. et al.), “transgender” plastic surgery, etc. Major iatrogenic consequences, which are generally final, can only be avoided through perfect knowledge of the anatomy. It is necessary to identify, for each of the 2 dorsal nerves of the clitoris, several segments, which each have a specific significance: the initial ischio-pubic segment, the ascending clitoral segment, the pre-symphysis (prepubic) segment, the corporeal clitoral dorsal segment and the termination at the glans. These various segments are separated by direction changes and actual kinking, which also deserve to be analysed in a specific study, especially the first during which we will observe how the cavernous nerve meets the dorsal nerve of the clitoris.
Get Clinical Tree app for offline access

The initial or ischio-pubic segment of the dorsal nerve of the clitoris is the superior division branche of the pudendal nerve of which it extends the direction, thus remaining in the fibrous pudendal canal with the artery and pudendal veins. It should be noted that this dorsal nerve of the clitoris is difficult to release in this initial segment, where it is routed against the ischio-pubic branch, below the fascia of the obturator internus, above the insertions of the deep fascia (superior fascia) of the urogenital diaphragm. It provides, at this level, the nerve of the external sphincter of the urethra, which will cross the above-mentioned fascia to join the sphincter fibres in the deep space of the perineum. Beyond the pudendal canal, the dorsal nerve of the clitoris will cross the pudendal artery, which will be in the more medial position. It surfaces by crossing through the superior fascia of the urogenital diaphragm and penetrates the deep space of the perineum, where it becomes accessible for perineal dissection. It may then, depending on the situation, remain above the inferior fascia of the urogenital diaphragm or, on the other hand, resurface by crossing through this fascia (Fig. 8.1). This penetration has been the subject of recent studies (A. Vaze et al.): according to these authors, it is located, on average, at 2 cm, 7 from the external orifice of the urethra. In both cases, the nerve will continue its forward and inward diagonal route towards the inferior branch of the pubis, which shelters and protects it and to which it is closely connected. At the inferior edge of this branch, a more or less deep groove can be observed. This groove has been described by Sedy J et al. as follows: the groove of the dorsal nerve of the clitoris (nearly 70 % of cases) is more or less marked, 15.8 mm long on average and even extends, according to these authors, at the inferior part of the ventral surface of the pubis. According to Sedy, this protective groove, which contains the nerve (which is often covered with a fibrous tissue), is as important as the pudendal canal because, in some cases, such as the latter, it can be too narrow and become a site of nerve compression (for cyclists in particular!), the consequence being a “syndrome of the dorsal nerve” (slightly different from the “pudendal nerve entrapment syndrome” and involving evocative symptoms such as an erectile malfunction). In order to meet the clitoris, the nerve finally reaches the inferior edge of the body of the pubis and its very dense prepubic fibrous coating. More precisely, it appears in the lateral part of the infra-pubic region, in front of the transverse perineal ligament (Henlé’s or Krause’s ligament), below the caudal symphysis edge (inferior edge), coated with the significant fibrous layers of the arcuate pubic ligament (Lauth’s ligament). Therefore, the nerve is in a very dense fibrous atmosphere, on which no author has insisted (except for Hruby S. et al., who described it in men) and which, however, plays a major protection role. Each of the 2 nerves will be wrapped at this level, in an actual protective sheath, a fibrous sleeve (with smooth internal wall), formed by the numerous fibrous components which surround the infra-pubic region. In some cases, certain nerves are wrapped in a fibrous canal formed by the duplication of the arcuate pubic ligament or even in a tunnel duplicated from the pre-symphysis tissue. The incision of the most superficial lamina of this envelope releases the nerve, which then seems to sprout out from an actual fibrous cone (Fig. 8.2). It should be noted that the homologous pudendal artery is also well protected, inside an underlying fibrous sleeve. The above details can be perfectly well observed by slightly tilting the clitoris, released from its pubic attachments, ventrally and backwards (Fig. 8.2). The thin subpubic urethral plate, which spreads out laterally up to the 2 nerves (which can be observed by transparency) must also be resected (Fig. 13.4).
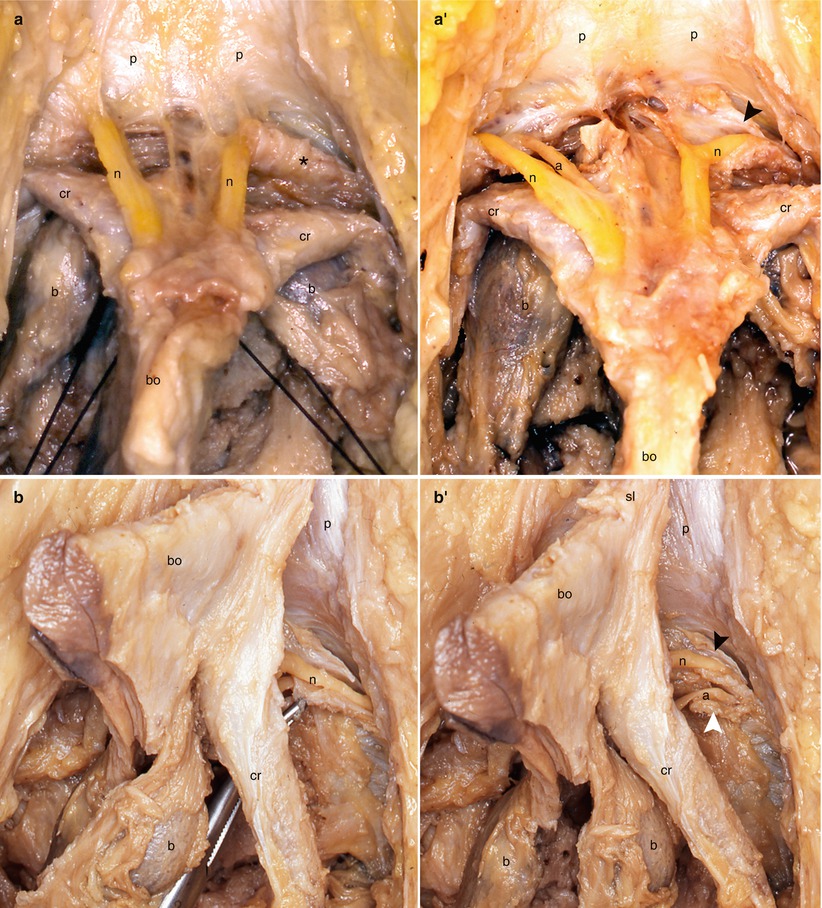
Fig. 8.2
The infra-pubic protective fibrous sheaths of the dorsal nerve and dorsal artery of clitoris. (a, a′) Views of the prepubic area (clitoral body retracted backwards and downwards). (b, b′) Side views of the bulbo-clitoral organ (detached from the pubic symphysis). (a) Note the left fibrous cone-shaped sheath , protecting the left dorsal nerve of clitoris. (a′) Note the opened fibrous sheaths. The opening of the left fibrous sheath (black arrowhead) shows the dorsal nerve of clitoris before it receives the cavernous nerve. (b) Note the opened fibrous sheath for the left dorsal nerve of clitoris (tracted by a forceps). (b′) Note the left opened fibrous sheaths of the nerve (black arrowhead) and of the artery (white arrowhead). a dorsal artery of clitoris, b bulb, bo body of clitoris, cr crus clitoridis, n dorsal nerve of clitoris, p pubis, sl suspensory ligament
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








